Overdiagnosis in cancer screening occurs when cancers are detected that would not have caused symptoms or harm during a person's lifetime. For example, prostate-specific antigen (PSA) tests for prostate cancer often identify slow-growing tumors that may never progress to a dangerous stage. These cases lead to unnecessary treatments, exposing patients to risks such as surgery complications and radiation side effects without real benefit. Breast cancer screening with mammography also demonstrates overdiagnosis by detecting ductal carcinoma in situ (DCIS), a non-invasive form of cancer that may not develop into invasive cancer. Studies estimate that up to 20-30% of breast cancers detected through mammography represent overdiagnosis. Overdiagnosis inflates cancer statistics, prompting overtreatment and increasing psychological stress for patients who might otherwise never have known about their condition.
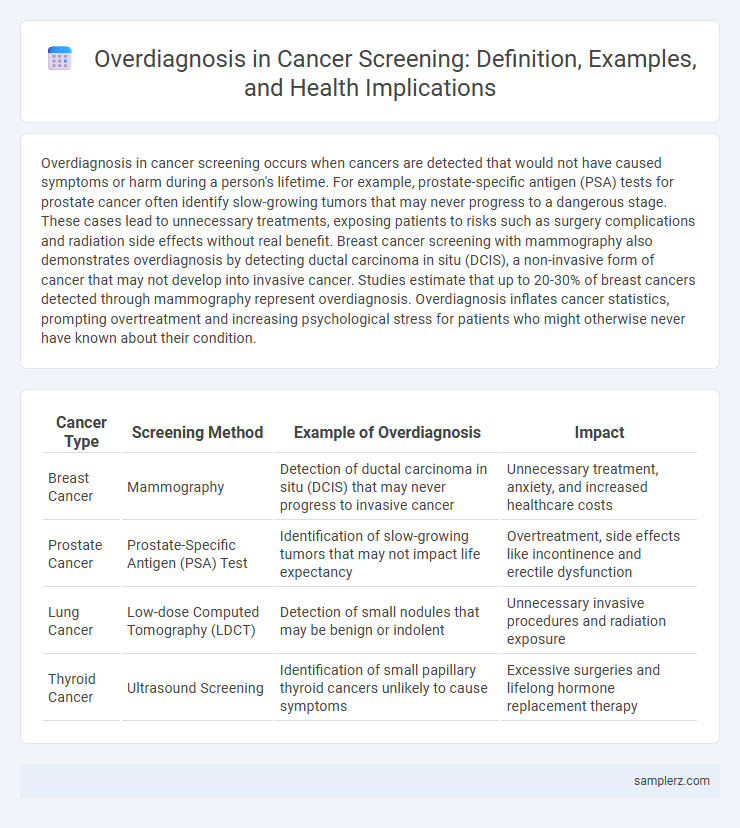
Table of Comparison
| Cancer Type | Screening Method | Example of Overdiagnosis | Impact |
|---|---|---|---|
| Breast Cancer | Mammography | Detection of ductal carcinoma in situ (DCIS) that may never progress to invasive cancer | Unnecessary treatment, anxiety, and increased healthcare costs |
| Prostate Cancer | Prostate-Specific Antigen (PSA) Test | Identification of slow-growing tumors that may not impact life expectancy | Overtreatment, side effects like incontinence and erectile dysfunction |
| Lung Cancer | Low-dose Computed Tomography (LDCT) | Detection of small nodules that may be benign or indolent | Unnecessary invasive procedures and radiation exposure |
| Thyroid Cancer | Ultrasound Screening | Identification of small papillary thyroid cancers unlikely to cause symptoms | Excessive surgeries and lifelong hormone replacement therapy |
Understanding Overdiagnosis in Cancer Screening
Overdiagnosis in cancer screening occurs when tests detect tumors that would never cause symptoms or harm during a patient's lifetime, leading to unnecessary treatments and anxiety. For instance, mammography can identify slow-growing breast cancers that may not progress, resulting in overtreatment. Understanding this phenomenon is crucial for balancing the benefits and harms of cancer screening programs and guiding evidence-based clinical decisions.
Common Cancers Prone to Overdiagnosis
Breast cancer and prostate cancer are common examples of cancers prone to overdiagnosis in screening programs. Mammography often detects ductal carcinoma in situ, which may never progress to invasive cancer, leading to unnecessary treatments. Prostate-specific antigen (PSA) testing frequently identifies indolent prostate tumors that would not cause symptoms or mortality if left untreated.
Overdiagnosis in Breast Cancer Screening
Overdiagnosis in breast cancer screening occurs when mammograms detect tumors that would not have caused symptoms or harm during a patient's lifetime. Studies estimate that 10-30% of breast cancers identified through routine screening are overdiagnosed, leading to unnecessary treatments such as surgery, radiation, or chemotherapy. This phenomenon highlights the importance of balancing early detection with the risks of overtreatment in breast cancer management.
Prostate Cancer: PSA Testing and Overdiagnosis
Prostate-Specific Antigen (PSA) testing often leads to overdiagnosis by detecting slow-growing prostate cancers that may never cause symptoms or affect a man's lifespan. This results in unnecessary treatments such as surgery or radiation, which carry risks of incontinence and erectile dysfunction. Studies indicate that up to 50% of prostate cancers detected through PSA screening represent overdiagnosis, highlighting the need for more targeted screening approaches.
Lung Cancer Screening: Balancing Benefits and Risks
Lung cancer screening using low-dose computed tomography (LDCT) can detect early-stage tumors but often leads to overdiagnosis by identifying non-aggressive lesions that may never cause symptoms or mortality. Studies indicate overdiagnosis rates in LDCT screening range from 18% to 30%, raising concerns about unnecessary treatments and psychological impact on patients. Balancing these risks with the mortality reduction benefit, estimated at 20% in high-risk populations, is critical for optimizing lung cancer screening protocols.
Thyroid Cancer: The Overdiagnosis Epidemic
Thyroid cancer screening has led to an overdiagnosis epidemic, with a dramatic rise in detected cases of small, indolent papillary thyroid tumors that may never cause symptoms or harm. Studies reveal that widespread use of ultrasounds and fine-needle biopsies often identifies subclinical lesions, inflating incidence rates without reducing mortality. This overdiagnosis results in unnecessary surgeries, exposure to potential complications, and psychological distress without clear benefits to patient survival.
Overdiagnosis in Colorectal Cancer Screening
Overdiagnosis in colorectal cancer screening occurs when asymptomatic, slow-growing polyps or tumors that would not cause harm during a patient's lifetime are detected and treated unnecessarily. Studies indicate this can lead to overtreatment, including invasive procedures and chemotherapy, exposing patients to risks without improving survival rates. Research shows that approximately 13-15% of colorectal cancer cases identified through screening may represent overdiagnosis.
Real-Life Case Studies: Impact of Overdiagnosis
Overdiagnosis in cancer screening is exemplified by studies on prostate-specific antigen (PSA) testing, where many men diagnosed with low-risk prostate cancer undergo unnecessary treatments that lead to significant side effects without improving survival rates. Similarly, breast cancer screening through mammography has revealed cases of ductal carcinoma in situ (DCIS), lesions that may never progress to invasive cancer yet result in aggressive interventions. These real-life case studies highlight the critical need for balanced screening protocols to minimize harm from overdiagnosis while maintaining early cancer detection benefits.
Consequences of Overdiagnosis for Patients and Healthcare
Overdiagnosis in cancer screening often leads to unnecessary treatments such as surgery, radiation, or chemotherapy, exposing patients to avoidable physical and psychological harm. These interventions increase healthcare costs and strain medical resources, diverting attention from patients with clinically significant cancers. Moreover, overdiagnosis can result in anxiety, reduced quality of life, and potential complications from invasive procedures despite the absence of life-threatening disease.
Reducing Overdiagnosis: Strategies and Recommendations
Reducing overdiagnosis in cancer screening involves adopting risk-based screening protocols that tailor the frequency and methods to individual patient risk profiles, minimizing unnecessary tests. Implementing shared decision-making between clinicians and patients enhances understanding of potential harms, helping to avoid excessive interventions. Integrating advanced imaging techniques and biomarkers improves specificity, decreasing false positives and overtreatment.
example of overdiagnosis in cancer screening Infographic
 samplerz.com
samplerz.com