Tachyphylaxis is a rapid decrease in the response to a medication after repeated doses over a short period. A common example in health is the use of nitroglycerin for angina pectoris, where continuous use leads to diminished vasodilatory effects. This phenomenon requires careful management to maintain therapeutic efficacy and avoid tolerance. Another notable example is with nasal decongestants like oxymetazoline, where frequent application results in rebound congestion due to receptor desensitization. In clinical practice, this limits the duration of use to prevent worsening symptoms. Understanding tachyphylaxis is crucial for optimizing drug regimens and ensuring patient safety.
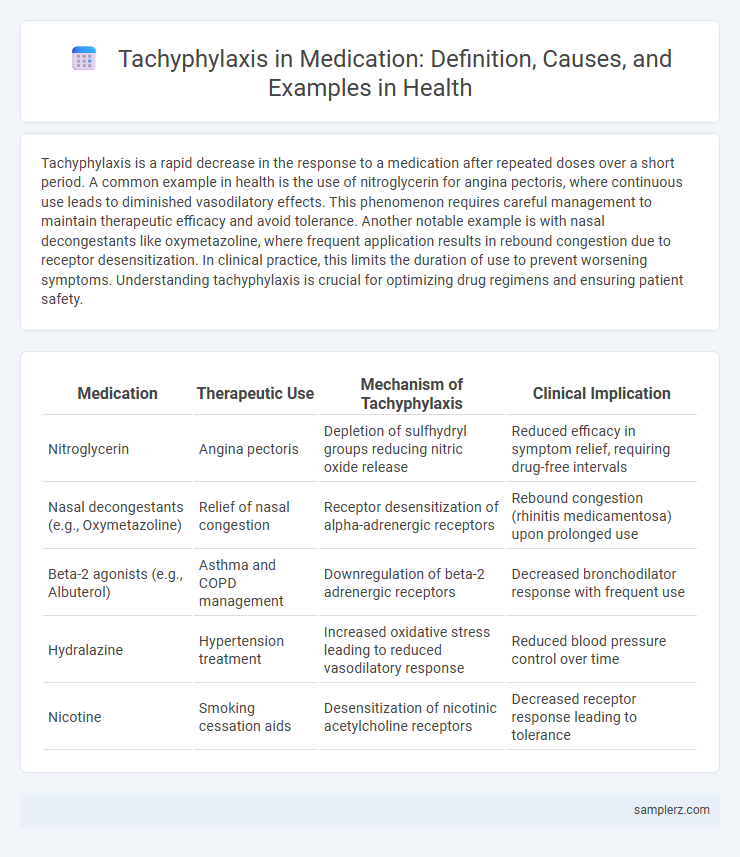
Table of Comparison
| Medication | Therapeutic Use | Mechanism of Tachyphylaxis | Clinical Implication |
|---|---|---|---|
| Nitroglycerin | Angina pectoris | Depletion of sulfhydryl groups reducing nitric oxide release | Reduced efficacy in symptom relief, requiring drug-free intervals |
| Nasal decongestants (e.g., Oxymetazoline) | Relief of nasal congestion | Receptor desensitization of alpha-adrenergic receptors | Rebound congestion (rhinitis medicamentosa) upon prolonged use |
| Beta-2 agonists (e.g., Albuterol) | Asthma and COPD management | Downregulation of beta-2 adrenergic receptors | Decreased bronchodilator response with frequent use |
| Hydralazine | Hypertension treatment | Increased oxidative stress leading to reduced vasodilatory response | Reduced blood pressure control over time |
| Nicotine | Smoking cessation aids | Desensitization of nicotinic acetylcholine receptors | Decreased receptor response leading to tolerance |
Understanding Tachyphylaxis in Medication
Tachyphylaxis occurs when the body's response to a medication rapidly diminishes after repeated doses, often seen with drugs like nitroglycerin and nasal decongestants. This phenomenon results from receptor desensitization or depletion of neurotransmitters, reducing drug efficacy over a short period. Understanding tachyphylaxis is critical for optimizing dosage regimens and preventing therapeutic failure in treatments involving beta-agonists or opioid analgesics.
Common Drugs Associated with Tachyphylaxis
Common drugs associated with tachyphylaxis include nasal decongestants like oxymetazoline and phenylephrine, which lose efficacy after prolonged use. Nitroglycerin, used for angina, demonstrates tachyphylaxis through reduced vasodilatory response with continuous exposure. Beta-2 agonists such as albuterol also exhibit diminished bronchodilator effects when used frequently in asthma management.
Mechanisms Behind Tachyphylaxis Development
Tachyphylaxis in medication frequently occurs with repeated use of nasal decongestants like oxymetazoline, where receptor desensitization reduces drug efficacy. The primary mechanism involves the rapid depletion of neurotransmitters or receptor downregulation, impairing normal signaling pathways. Adaptive cellular changes, such as receptor internalization and alterations in second messenger systems, further contribute to diminished drug response during continued exposure.
Clinical Presentation of Tachyphylaxis
Tachyphylaxis in medication presents clinically as a rapidly diminishing response to a drug following its repeated administration, often observed with nasal decongestants like oxymetazoline or beta-agonists such as albuterol. Patients typically report reduced efficacy within hours to days, manifesting as persistent symptoms despite adherence to prescribed doses. Physical signs may include rebound congestion or worsening bronchospasm, necessitating reassessment of therapeutic strategies.
Antidepressants and Tachyphylaxis: An Overview
Tachyphylaxis in antidepressants manifests as a rapid decrease in therapeutic response, often observed with selective serotonin reuptake inhibitors (SSRIs) such as fluoxetine and sertraline. This phenomenon may result from neurotransmitter receptor desensitization or alterations in serotonin transporter function, reducing drug efficacy. Clinicians monitor symptoms closely and may adjust treatment by switching antidepressants or incorporating augmentation strategies to overcome tachyphylaxis.
Tachyphylaxis in Antihistamine Therapy
Tachyphylaxis in antihistamine therapy occurs when repeated use of H1 receptor antagonists leads to a diminished therapeutic response, reducing effectiveness in alleviating allergic symptoms such as rhinitis and urticaria. This phenomenon is commonly observed with first-generation antihistamines like diphenhydramine, where receptor desensitization and downregulation limit histamine blockade. Managing tachyphylaxis involves drug rotation or dosage adjustments to maintain receptor sensitivity and optimize symptomatic relief.
Insulin and Tachyphylaxis in Diabetes Management
Tachyphylaxis in diabetes management often occurs with insulin therapy, where repeated exposure to insulin leads to diminished glucose-lowering effects. This phenomenon necessitates careful dose adjustments or switching insulin types to maintain glycemic control in patients with Type 1 or Type 2 diabetes. Monitoring insulin sensitivity and resistance markers is essential to optimize therapeutic outcomes and prevent complications related to tachyphylaxis.
Strategies to Manage Medication Tachyphylaxis
Medication tachyphylaxis, characterized by a rapid decrease in drug response, often occurs with repeated use of nasal decongestants like oxymetazoline. Effective management strategies include drug holidays, dose reduction, and alternating medications to restore drug sensitivity. Monitoring patient response and adjusting treatment protocols accordingly are critical for preventing tolerance and enhancing therapeutic outcomes.
Preventing Tachyphylaxis in Long-Term Treatment
Tachyphylaxis often occurs with long-term use of nasal decongestants like oxymetazoline, where receptor desensitization reduces drug efficacy. Preventing tachyphylaxis involves implementing drug holidays, limiting continuous use to a few days, and rotating medications to maintain receptor responsiveness. Monitoring patient response and adjusting dosage schedules are crucial strategies for sustaining therapeutic effects and minimizing tolerance in chronic treatments.
Future Research on Tachyphylaxis and Drug Effectiveness
Future research on tachyphylaxis aims to identify molecular mechanisms responsible for rapid drug tolerance, enhancing personalized medicine approaches. Investigating genetic markers linked to tachyphylaxis can improve prediction of patient responses to medications such as beta-agonists and nitrates. Advances in pharmacogenomics and real-time monitoring technologies promise to optimize drug dosing schedules, minimizing loss of effectiveness.
example of tachyphylaxis in medication Infographic
 samplerz.com
samplerz.com