Tachyphylaxis is a rapid decrease in the response to a drug after repeated administration, which results in diminished therapeutic effects. A common example in the health field is the use of nasal decongestants such as oxymetazoline. Patients often experience reduced nasal airway relief after continuous use for more than three days, as the receptors become desensitized. In clinical practice, tachyphylaxis presents a challenge in managing chronic conditions requiring sustained drug therapy. Another example involves beta-2 agonists used in asthma treatment, where repeated doses can lead to decreased bronchodilator effectiveness. Understanding the mechanisms behind tachyphylaxis supports better therapeutic strategies and improves patient outcomes by preventing drug tolerance.
Table of Comparison
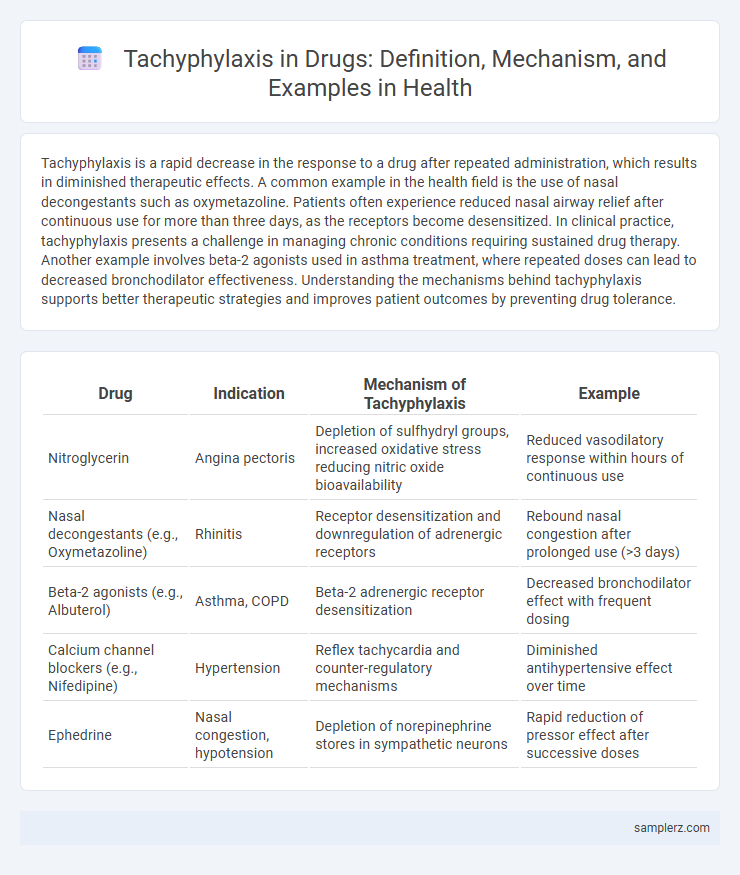
| Drug | Indication | Mechanism of Tachyphylaxis | Example |
|---|---|---|---|
| Nitroglycerin | Angina pectoris | Depletion of sulfhydryl groups, increased oxidative stress reducing nitric oxide bioavailability | Reduced vasodilatory response within hours of continuous use |
| Nasal decongestants (e.g., Oxymetazoline) | Rhinitis | Receptor desensitization and downregulation of adrenergic receptors | Rebound nasal congestion after prolonged use (>3 days) |
| Beta-2 agonists (e.g., Albuterol) | Asthma, COPD | Beta-2 adrenergic receptor desensitization | Decreased bronchodilator effect with frequent dosing |
| Calcium channel blockers (e.g., Nifedipine) | Hypertension | Reflex tachycardia and counter-regulatory mechanisms | Diminished antihypertensive effect over time |
| Ephedrine | Nasal congestion, hypotension | Depletion of norepinephrine stores in sympathetic neurons | Rapid reduction of pressor effect after successive doses |
Understanding Tachyphylaxis: Definition and Mechanism
Tachyphylaxis refers to a rapidly diminishing response to a drug after its initial administration, often observed with medications such as nitroglycerin and nasal decongestants like oxymetazoline. This phenomenon occurs due to receptor desensitization or depletion of neurotransmitters, leading to reduced drug efficacy over time. Understanding the cellular mechanisms behind tachyphylaxis is crucial for optimizing therapeutic strategies and preventing treatment failure in clinical practice.
Common Drugs Associated with Tachyphylaxis
Common drugs associated with tachyphylaxis include nitroglycerin, beta-agonists like albuterol, and decongestants such as oxymetazoline. Repeated use of nitroglycerin patches can lead to decreased efficacy in angina management due to rapid tolerance development. Albuterol inhalers often show reduced bronchodilator response during acute asthma exacerbations as a result of receptor desensitization.
Antihistamines: Rapid Tolerance Development
Tachyphylaxis in antihistamines manifests as a rapid decrease in drug efficacy, often seen within days of continuous use to relieve allergic symptoms. This tolerance development results from the desensitization of histamine H1 receptors, reducing the drug's ability to block histamine-mediated responses. Clinical studies highlight the diminished antipruritic and anti-inflammatory effects of first-generation antihistamines, necessitating dosage adjustment or drug rotation for sustained allergy management.
Nasal Decongestants: Classic Tachyphylaxis Example
Nasal decongestants such as oxymetazoline and phenylephrine display classic tachyphylaxis, where repeated intranasal use leads to diminished vasoconstrictive effects and rebound nasal congestion. This rapid tolerance occurs due to receptor desensitization and downregulation of alpha-adrenergic receptors in the nasal mucosa. Limiting use to three consecutive days is recommended to prevent tachyphylaxis and avoid chronic rhinitis.
Nitrate Medications and Diminished Response
Tachyphylaxis in nitrate medications occurs when repeated use leads to a diminished response, reducing their effectiveness in treating conditions such as angina pectoris. This phenomenon results from cellular mechanisms like nitrate tolerance, where continuous exposure decreases nitric oxide bioavailability and impairs vasodilation. Understanding nitrate tachyphylaxis is critical for optimizing dosing schedules and preventing therapeutic failure in cardiovascular management.
Antidepressants and Tachyphylaxis Phenomena
Tachyphylaxis in antidepressants occurs when patients experience a rapid decrease in drug efficacy, often seen with selective serotonin reuptake inhibitors (SSRIs) after weeks of treatment. This phenomenon involves receptor desensitization and neurotransmitter system adaptations, leading to diminished clinical response despite continued medication use. Understanding tachyphylaxis is crucial for optimizing antidepressant therapy and managing treatment-resistant depression.
Insulin Therapy: Loss of Effectiveness Over Time
Tachyphylaxis in insulin therapy occurs when patients experience a diminished response to insulin after prolonged use, leading to reduced glucose control despite consistent dosing. This phenomenon is often linked to receptor downregulation or antibody formation against insulin, resulting in decreased drug efficacy. Monitoring blood glucose levels and adjusting insulin regimens are essential to managing this loss of effectiveness and maintaining optimal therapeutic outcomes.
Beta-Agonists in Asthma Management
Tachyphylaxis in asthma management often occurs with repeated use of beta-agonists like albuterol, leading to a diminished bronchodilator response over time. This desensitization results from beta-2 adrenergic receptor downregulation and reduced cyclic AMP production. Clinicians must monitor patients closely and consider combination therapy with corticosteroids to mitigate tachyphylaxis effects in chronic asthma treatment.
Strategies to Prevent or Manage Tachyphylaxis
Tachyphylaxis frequently occurs with drugs such as nitrates and beta-agonists, where rapid tolerance diminishes therapeutic efficacy. Strategies to prevent or manage tachyphylaxis include drug holidays, dose escalation, and rotating medications to maintain receptor sensitivity. Clinicians also employ combination therapies and monitor patient responses closely to adjust treatment regimens effectively.
Clinical Significance and Patient Considerations
Tachyphylaxis to nitroglycerin in angina patients results in rapid tolerance, reducing drug efficacy and necessitating intermittent dosing schedules to maintain therapeutic benefits. Clinicians must evaluate patients for diminishing responses to repeated doses and adjust treatment plans accordingly to prevent breakthrough symptoms. Patient education on adherence to loading and drug-free intervals is critical to optimize symptom control and avoid adverse cardiovascular events.
example of tachyphylaxis in drug Infographic
 samplerz.com
samplerz.com