Iatrogenesis in health refers to any adverse condition or complication induced unintentionally by medical treatment or diagnostic procedures. One common example is antibiotic-associated diarrhea, which occurs when the use of antibiotics disrupts the natural balance of gut microbiota, leading to gastrointestinal issues such as Clostridium difficile infection. This condition illustrates how therapeutic interventions can inadvertently cause harm despite their intended beneficial effects. Another example of iatrogenic effects is radiation-induced skin damage during cancer therapy. Radiation treatment aimed at destroying malignant cells can also harm surrounding healthy tissue, resulting in symptoms like redness, blistering, and long-term scarring. These examples reflect the importance of careful management, monitoring, and balancing the risks and benefits of medical interventions to minimize iatrogenic harm.
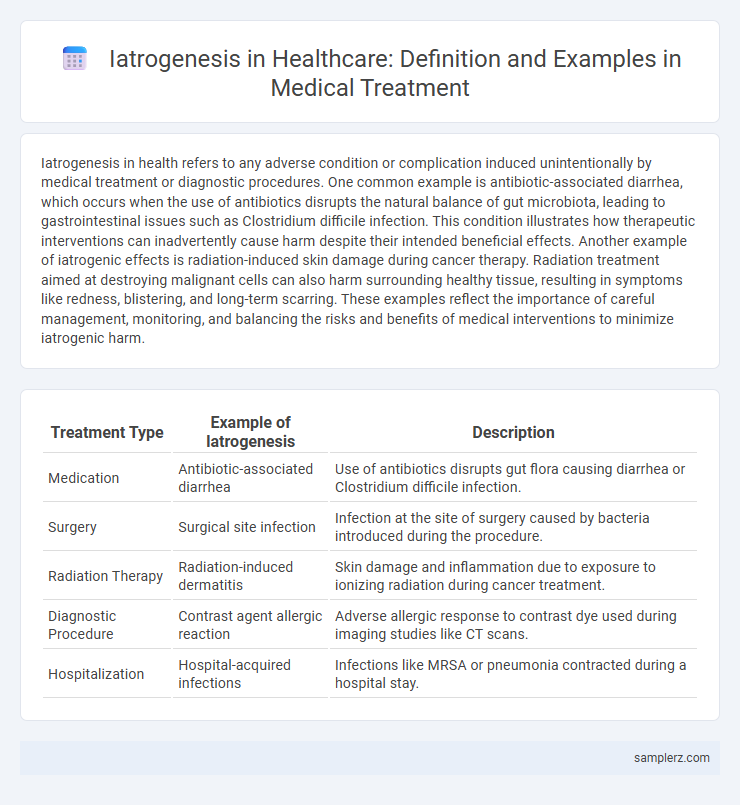
Table of Comparison
| Treatment Type | Example of Iatrogenesis | Description |
|---|---|---|
| Medication | Antibiotic-associated diarrhea | Use of antibiotics disrupts gut flora causing diarrhea or Clostridium difficile infection. |
| Surgery | Surgical site infection | Infection at the site of surgery caused by bacteria introduced during the procedure. |
| Radiation Therapy | Radiation-induced dermatitis | Skin damage and inflammation due to exposure to ionizing radiation during cancer treatment. |
| Diagnostic Procedure | Contrast agent allergic reaction | Adverse allergic response to contrast dye used during imaging studies like CT scans. |
| Hospitalization | Hospital-acquired infections | Infections like MRSA or pneumonia contracted during a hospital stay. |
Common Examples of Iatrogenesis in Medical Treatments
Common examples of iatrogenesis in medical treatments include medication errors such as incorrect dosages or harmful drug interactions, surgical complications like infections or unintended tissue damage, and adverse reactions to anesthesia. Diagnostic procedures can also cause iatrogenic harm through unnecessary biopsies leading to bleeding or pneumothorax during central line placement. These instances highlight the critical importance of careful clinical judgment and patient monitoring to minimize preventable medical injuries.
Medication-Induced Iatrogenic Complications
Medication-induced iatrogenic complications commonly occur due to adverse drug reactions, dosage errors, or dangerous drug interactions, leading to conditions such as kidney failure, gastrointestinal bleeding, or cardiac arrhythmias. Elderly patients and those with multiple comorbidities are particularly vulnerable to these complications, highlighting the importance of careful medication management and monitoring. Health systems report that polypharmacy is a significant risk factor, contributing to increased hospitalizations and healthcare costs related to iatrogenic events.
Surgical Procedures Leading to Iatrogenic Harm
Surgical procedures can result in iatrogenic harm through unintended damage to surrounding tissues or organs, such as nerve injury during orthopedic surgery or bowel perforation in abdominal operations. Postoperative complications like infections, bleeding, or anesthesia-related adverse effects also exemplify iatrogenesis in surgical treatment. Identifying and minimizing these risks is crucial for enhancing patient safety and surgical outcomes.
Diagnostic Errors and Iatrogenic Outcomes
Diagnostic errors, such as misinterpretation of imaging or laboratory results, can lead to iatrogenic outcomes including unnecessary surgeries or harmful medication regimens. These errors contribute to patient harm by delaying appropriate treatment and increasing healthcare costs. Effective strategies to reduce diagnostic inaccuracies involve improved clinician training and the integration of advanced decision-support technologies.
Iatrogenic Infections: Causes and Prevention
Iatrogenic infections occur when pathogens are introduced to patients during medical procedures, often due to inadequate sterilization of surgical instruments or improper hand hygiene by healthcare providers. Common causes include contaminated catheters, ventilators, and surgical sites, which can result in bloodstream infections, pneumonia, or surgical site infections. Preventing these infections relies on strict adherence to infection control protocols, use of sterile equipment, and ongoing staff training on hygiene practices in healthcare settings.
Adverse Drug Reactions as Iatrogenic Events
Adverse Drug Reactions (ADRs) represent a significant example of iatrogenesis in medical treatment, occurring when prescribed medications cause unintended harmful effects. Common ADRs include allergic reactions, drug interactions, and organ toxicity, which can complicate patient recovery and increase healthcare costs. Monitoring pharmacovigilance and implementing personalized medicine strategies help reduce the incidence of these iatrogenic events.
Medical Device-Related Iatrogenesis
Medical device-related iatrogenesis occurs when medical equipment such as catheters, ventilators, or implants cause unintended harm to patients. Common examples include infections from indwelling catheters, pressure ulcers from improper ventilator settings, and tissue damage due to implant malfunction. Monitoring device usage protocols and maintaining sterilization standards are critical to minimizing these adverse outcomes in healthcare settings.
Iatrogenesis from Over-Treatment and Polypharmacy
Over-treatment and polypharmacy significantly contribute to iatrogenesis, causing adverse drug reactions, increased hospitalizations, and higher healthcare costs. Elderly patients with multiple chronic conditions are particularly vulnerable due to the complex medication regimens and potential drug interactions. Recognizing and reducing unnecessary treatments helps mitigate risks and improve patient safety outcomes.
Psychological Effects of Iatrogenic Injury
Iatrogenesis in treatment often leads to psychological effects such as anxiety, depression, and post-traumatic stress disorder (PTSD) in patients experiencing medical errors or adverse events. These psychological consequences can result from prolonged hospitalization, invasive procedures, or misdiagnosis, significantly impacting patients' mental health and quality of life. Effective communication and supportive mental health interventions are essential to mitigate the psychological burden associated with iatrogenic injury.
Strategies to Reduce Iatrogenic Risks in Healthcare
Implementing comprehensive medication reviews and enhancing electronic health record integration significantly reduce iatrogenic risks by minimizing adverse drug interactions and errors. Training healthcare professionals on updated clinical protocols and promoting patient engagement in treatment decisions improve early detection of complications. Utilizing standardized checklists and fostering multidisciplinary communication streamline care processes, further decreasing the incidence of iatrogenic harm in medical treatments.
example of iatrogenesis in treatment Infographic
 samplerz.com
samplerz.com