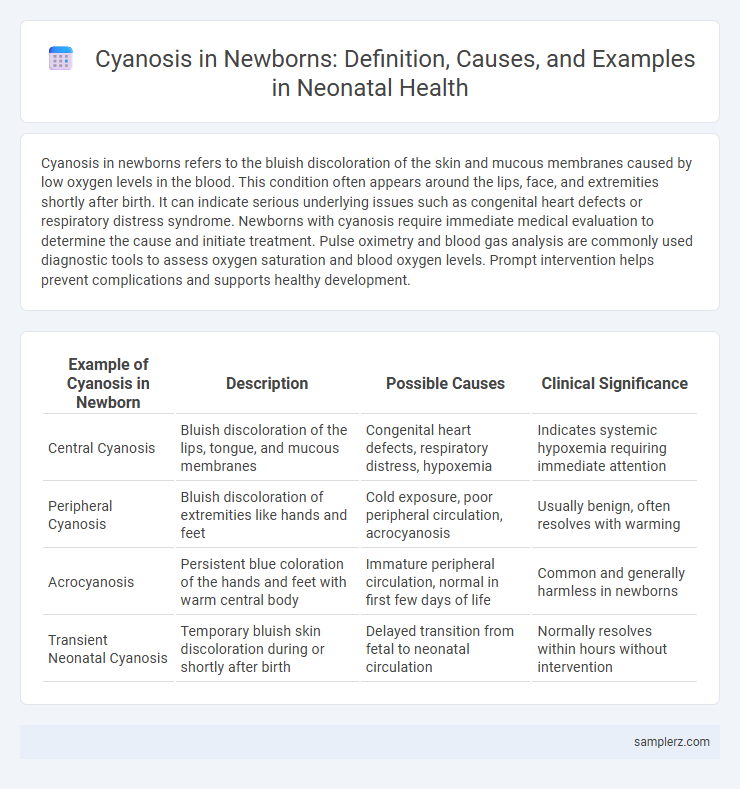
Cyanosis in newborns refers to the bluish discoloration of the skin and mucous membranes caused by low oxygen levels in the blood. This condition often appears around the lips, face, and extremities shortly after birth. It can indicate serious underlying issues such as congenital heart defects or respiratory distress syndrome. Newborns with cyanosis require immediate medical evaluation to determine the cause and initiate treatment. Pulse oximetry and blood gas analysis are commonly used diagnostic tools to assess oxygen saturation and blood oxygen levels. Prompt intervention helps prevent complications and supports healthy development.
Table of Comparison
| Example of Cyanosis in Newborn | Description | Possible Causes | Clinical Significance |
|---|---|---|---|
| Central Cyanosis | Bluish discoloration of the lips, tongue, and mucous membranes | Congenital heart defects, respiratory distress, hypoxemia | Indicates systemic hypoxemia requiring immediate attention |
| Peripheral Cyanosis | Bluish discoloration of extremities like hands and feet | Cold exposure, poor peripheral circulation, acrocyanosis | Usually benign, often resolves with warming |
| Acrocyanosis | Persistent blue coloration of the hands and feet with warm central body | Immature peripheral circulation, normal in first few days of life | Common and generally harmless in newborns |
| Transient Neonatal Cyanosis | Temporary bluish skin discoloration during or shortly after birth | Delayed transition from fetal to neonatal circulation | Normally resolves within hours without intervention |
Introduction to Cyanosis in Newborns
Cyanosis in newborns is characterized by a bluish discoloration of the skin and mucous membranes due to inadequate oxygenation of the blood. This condition may indicate underlying respiratory or cardiac complications such as congenital heart defects or pulmonary disorders. Early recognition and prompt evaluation are critical to prevent hypoxic damage and ensure appropriate treatment.
Types of Cyanosis Observed in Newborns
Peripheral cyanosis in newborns presents as bluish discoloration of the hands and feet due to slowed peripheral circulation, while central cyanosis affects the tongue, lips, and mucous membranes caused by inadequate oxygenation of arterial blood. Differential diagnosis includes acrocyanosis, a benign and transient form common in healthy neonates, and pathological cyanosis linked to congenital heart defects such as Tetralogy of Fallot or pulmonary hypertension. Pulse oximetry and arterial blood gas analysis are critical diagnostic tools to distinguish between these types and guide immediate clinical interventions.
Common Causes of Cyanosis in Newborn Infants
Cyanosis in newborn infants often results from congenital heart defects such as tetralogy of Fallot and transposition of the great arteries, which impair oxygenated blood flow. Respiratory conditions like neonatal pneumonia or meconium aspiration syndrome also commonly cause cyanosis by limiting oxygen exchange in the lungs. Persistent pulmonary hypertension of the newborn (PPHN) represents another critical cause, where high pulmonary vascular resistance leads to decreased oxygen saturation.
Central vs Peripheral Cyanosis: Key Differences
Central cyanosis in newborns manifests as a bluish discoloration of the tongue and lips, indicating low oxygen saturation in arterial blood and potentially signaling congenital heart defects or respiratory distress. Peripheral cyanosis, on the other hand, appears as bluish tint in the extremities like hands and feet due to slowed blood flow or cold exposure, often without significant systemic hypoxia. Differentiating between central and peripheral cyanosis is crucial for timely diagnosis and intervention, with pulse oximetry and physical examination playing key roles in clinical assessment.
Clinical Signs of Cyanosis in Neonates
Clinical signs of cyanosis in newborns include bluish discoloration of the lips, tongue, and mucous membranes, indicating insufficient oxygenation of the blood. Peripheral cyanosis presents as bluish extremities, often less concerning unless it persists beyond the first 24 hours or is accompanied by respiratory distress. Central cyanosis, a more critical sign, requires immediate evaluation for congenital heart defects or pulmonary conditions.
Notable Examples of Cyanosis in Newborn Cases
Notable examples of cyanosis in newborn cases include congenital heart defects such as Tetralogy of Fallot and transposition of the great arteries, which lead to inadequate oxygenation of blood. Persistent pulmonary hypertension of the newborn (PPHN) also presents with cyanosis due to high pulmonary vascular resistance, restricting blood flow to the lungs. Early detection and intervention in these conditions are critical for preventing severe hypoxia and improving neonatal outcomes.
Diagnosis of Cyanosis in Newborns: Step-by-Step Guide
Diagnosis of cyanosis in newborns involves assessing skin and mucous membrane color under natural light, measuring oxygen saturation using pulse oximetry, and conducting arterial blood gas analysis to determine hypoxemia severity. Differential diagnosis includes distinguishing between central and peripheral cyanosis by evaluating systemic oxygenation and circulation status. Echocardiography and chest X-ray may be employed to identify underlying cardiac or pulmonary causes contributing to neonatal cyanosis.
Management and Treatment Options for Neonatal Cyanosis
Management of neonatal cyanosis involves immediate assessment of airway, breathing, and circulation to ensure adequate oxygenation. Treatment options include supplemental oxygen therapy, addressing underlying causes such as congenital heart defects through surgical intervention, and use of medications like prostaglandin E1 to maintain ductal patency in critical heart lesions. Continuous monitoring with pulse oximetry and arterial blood gases is essential for guiding treatment efficacy and patient stability.
Potential Complications Linked to Cyanosis in Newborns
Cyanosis in newborns, characterized by a bluish discoloration of the skin and mucous membranes, often signals underlying hypoxemia that can lead to severe complications such as persistent pulmonary hypertension of the newborn (PPHN) and congenital heart defects like Tetralogy of Fallot. Untreated cyanosis increases the risk of cerebral hypoxia, resulting in long-term neurodevelopmental deficits and potential organ dysfunction. Early diagnosis through pulse oximetry and prompt intervention with oxygen therapy or surgical correction is critical to reduce morbidity and mortality associated with cyanosis in neonates.
When to Seek Emergency Care for Newborn Cyanosis
Newborn cyanosis, characterized by a bluish discoloration of the skin, lips, or nail beds, requires immediate medical attention if it occurs during feeding, crying, or at rest, indicating potential respiratory or cardiac distress. Seek emergency care when cyanosis is accompanied by rapid breathing, grunting, lethargy, or poor feeding, as these symptoms may signal serious conditions such as congenital heart defects or respiratory infections. Timely intervention by pediatric healthcare providers is crucial to prevent complications and ensure optimal newborn health outcomes.
example of cyanosis in newborn Infographic
 samplerz.com
samplerz.com