Nosocomial infections, also known as hospital-acquired infections, occur during a patient's stay in a healthcare facility. An example includes methicillin-resistant Staphylococcus aureus (MRSA) infections, which are commonly spread through contaminated medical equipment or contact with infected healthcare workers. These infections significantly impact hospital data, showing increased patient morbidity and extended lengths of stay. Another example of a nosocomial infection is catheter-associated urinary tract infections (CAUTIs), frequently documented in hospital records. Data indicates that improper catheter care or prolonged catheter use contributes to these infections. Tracking and analysis of such cases help hospitals implement targeted infection control measures to reduce incidence rates.
Table of Comparison
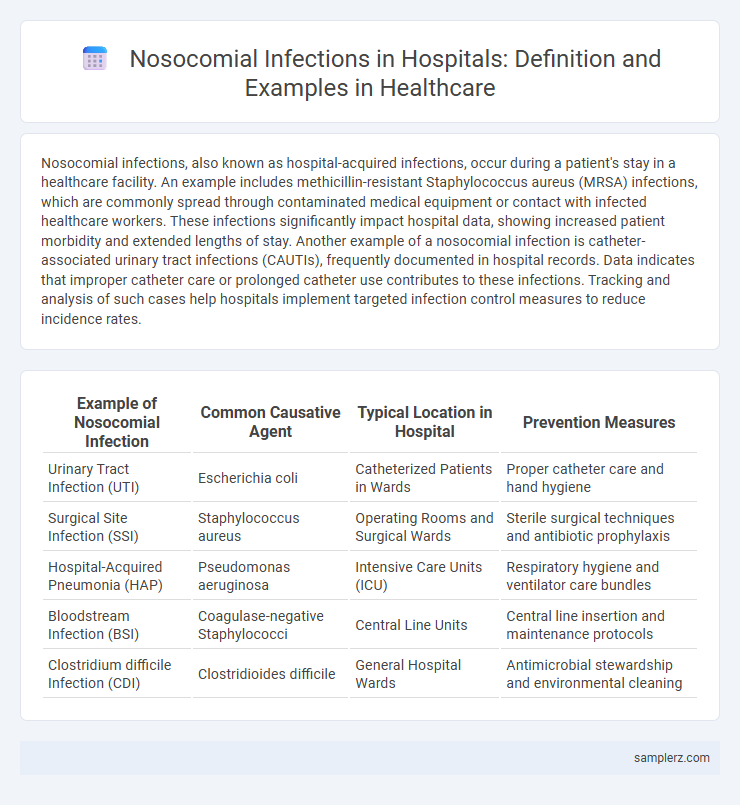
| Example of Nosocomial Infection | Common Causative Agent | Typical Location in Hospital | Prevention Measures |
|---|---|---|---|
| Urinary Tract Infection (UTI) | Escherichia coli | Catheterized Patients in Wards | Proper catheter care and hand hygiene |
| Surgical Site Infection (SSI) | Staphylococcus aureus | Operating Rooms and Surgical Wards | Sterile surgical techniques and antibiotic prophylaxis |
| Hospital-Acquired Pneumonia (HAP) | Pseudomonas aeruginosa | Intensive Care Units (ICU) | Respiratory hygiene and ventilator care bundles |
| Bloodstream Infection (BSI) | Coagulase-negative Staphylococci | Central Line Units | Central line insertion and maintenance protocols |
| Clostridium difficile Infection (CDI) | Clostridioides difficile | General Hospital Wards | Antimicrobial stewardship and environmental cleaning |
Common Types of Nosocomial Infections in Hospitals
Common types of nosocomial infections in hospitals include bloodstream infections, surgical site infections, urinary tract infections, and pneumonia. These infections are primarily caused by multidrug-resistant organisms such as MRSA, Clostridium difficile, and Pseudomonas aeruginosa. Strict adherence to infection control protocols and antimicrobial stewardship is essential to reduce the incidence of these hospital-acquired infections.
Most Frequent Sources of Hospital-Acquired Infections
The most frequent sources of nosocomial infections in hospitals include contaminated medical devices such as catheters and ventilators, which serve as common entry points for pathogens. Healthcare workers' hands often act as vectors, transferring bacteria like Staphylococcus aureus and Clostridium difficile between patients. Additionally, surgical sites and bloodstream infections frequently arise from lapses in sterile techniques and inadequate disinfection protocols.
Examples of Bacterial Nosocomial Infections
Common examples of bacterial nosocomial infections in hospitals include Methicillin-resistant Staphylococcus aureus (MRSA), Clostridium difficile causing severe diarrhea, and Pseudomonas aeruginosa associated with bloodstream infections. These pathogens often thrive in intensive care units and surgical sites due to invasive procedures and prolonged hospital stays. Effective infection control protocols and antibiotic stewardship are critical to reducing the incidence and spread of these bacterial infections.
Viral Infections Acquired in Hospital Settings
Nosocomial viral infections commonly acquired in hospital settings include respiratory syncytial virus (RSV), influenza, and norovirus, which pose significant risks to immunocompromised patients. These infections often spread through contaminated surfaces, airborne droplets, and close contact in crowded hospital wards, leading to increased morbidity and extended hospital stays. Implementing strict infection control protocols such as hand hygiene, isolation procedures, and vaccination for healthcare workers is critical to reducing the incidence of hospital-acquired viral infections.
Fungal Nosocomial Infections in Healthcare Facilities
Fungal nosocomial infections, such as candidemia and invasive aspergillosis, pose significant risks in healthcare facilities, particularly among immunocompromised patients. Candida species, especially Candida albicans and Candida auris, are common culprits causing bloodstream infections linked to indwelling medical devices and prolonged antibiotic use. Aspergillus spores, often found in hospital ventilation systems or construction areas, contribute to respiratory infections that complicate patient outcomes and increase hospital stays.
Medical Procedures Associated with Nosocomial Risks
Surgical procedures such as orthopedic implantations and catheter insertions are common medical interventions associated with nosocomial infections in hospitals. Ventilator-associated pneumonia frequently occurs in intensive care units due to prolonged mechanical ventilation. Central line-associated bloodstream infections (CLABSIs) remain significant risks linked to intravenous catheter use in inpatient settings.
Patient Populations Most Vulnerable to Nosocomial Infections
Immunocompromised patients, such as those undergoing chemotherapy or organ transplantation, face a significantly higher risk of nosocomial infections due to weakened immune defenses. Elderly individuals and neonates are also highly susceptible because of their reduced immune response and frequent exposure to invasive procedures. Intensive care unit (ICU) patients with prolonged hospital stays and multiple invasive devices exhibit increased vulnerability to hospital-acquired infections like ventilator-associated pneumonia and catheter-related bloodstream infections.
Real Cases: Notable Nosocomial Outbreaks in Hospitals
The 2011 California outbreak of methicillin-resistant Staphylococcus aureus (MRSA) in a Los Angeles hospital highlighted the critical challenges of infection control in healthcare settings. Similarly, the 2015 Ebola virus transmission within Dallas Presbyterian Hospital underscored the vulnerability of hospital environments to high-risk infectious agents. These cases emphasize the importance of stringent hygiene protocols, rapid detection, and isolation measures to prevent nosocomial infections.
Shared Equipment as a Source of Nosocomial Pathogens
Shared medical equipment such as stethoscopes, blood pressure cuffs, and thermometers can serve as significant sources of nosocomial pathogens within hospitals. Contamination of these devices with bacteria like MRSA and Clostridium difficile facilitates cross-transmission of infections among patients. Rigorous disinfection protocols and single-patient use policies are essential to minimize the risk of healthcare-associated infections linked to shared equipment.
Environmental Factors Contributing to Nosocomial Infections
Contaminated hospital surfaces such as bed rails, medical equipment, and door handles serve as significant reservoirs for pathogenic microorganisms, facilitating the transmission of nosocomial infections. Inadequate ventilation systems and improper sterilization of surgical instruments further exacerbate microbial contamination, increasing infection risks for vulnerable patients. High patient density and overcrowded wards also contribute to the spread of airborne and contact-transmitted hospital-acquired infections.
example of nosocomial in hospital Infographic
 samplerz.com
samplerz.com