Melaena is a clinical sign indicating bleeding within the gastrointestinal (GI) tract, characterized by black, tarry stools due to the presence of digested blood. It commonly arises from upper GI sources such as peptic ulcers, esophageal varices, or gastritis, where bleeding occurs and the blood undergoes digestion as it passes through the intestines. Diagnostic approaches often include endoscopy to identify the bleeding site and laboratory tests to assess anemia and hemodynamic status. In the context of GI diseases, melaena serves as an alarming symptom that requires prompt medical evaluation. For instance, peptic ulcer disease produces mucosal erosions that may bleed intermittently, resulting in melaena. Esophageal varices, often related to portal hypertension in liver cirrhosis, pose a risk of massive upper GI bleeding manifesting as melaena, necessitating urgent intervention to prevent morbidity.
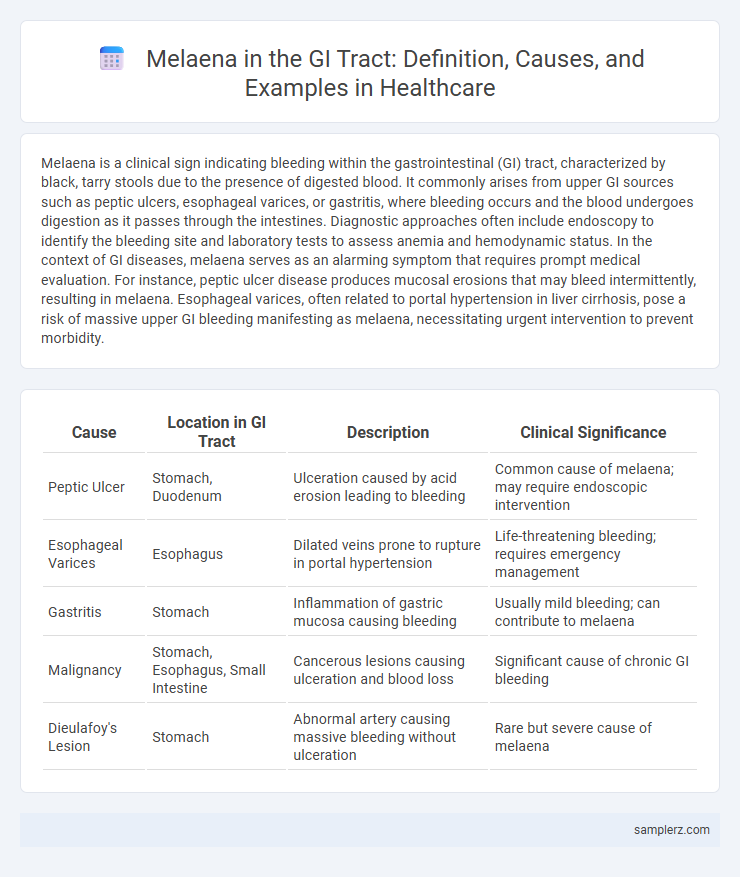
Table of Comparison
| Cause | Location in GI Tract | Description | Clinical Significance |
|---|---|---|---|
| Peptic Ulcer | Stomach, Duodenum | Ulceration caused by acid erosion leading to bleeding | Common cause of melaena; may require endoscopic intervention |
| Esophageal Varices | Esophagus | Dilated veins prone to rupture in portal hypertension | Life-threatening bleeding; requires emergency management |
| Gastritis | Stomach | Inflammation of gastric mucosa causing bleeding | Usually mild bleeding; can contribute to melaena |
| Malignancy | Stomach, Esophagus, Small Intestine | Cancerous lesions causing ulceration and blood loss | Significant cause of chronic GI bleeding |
| Dieulafoy's Lesion | Stomach | Abnormal artery causing massive bleeding without ulceration | Rare but severe cause of melaena |
Understanding Melaena: Definition and Clinical Importance
Melaena refers to the passage of black, tarry stools indicative of upper gastrointestinal bleeding, commonly originating from sources such as gastric ulcers or esophageal varices. Identifying melaena is crucial for clinicians as it signals significant hemorrhage in the GI tract requiring urgent diagnostic evaluation and intervention. Early recognition and management of melaena improve patient outcomes by preventing complications associated with severe blood loss and hemodynamic instability.
Common Causes of Melaena in the GI Tract
Melaena, characterized by black tarry stools, commonly results from upper gastrointestinal bleeding sources such as peptic ulcers, gastritis, and esophageal varices. Other frequent causes include Mallory-Weiss tears and malignancies of the stomach or duodenum. Accurate diagnosis often relies on endoscopic evaluation to identify the bleeding site within the GI tract.
Upper Gastrointestinal Bleeding: Typical Melaena Examples
Typical melaena examples in upper gastrointestinal bleeding include bleeding from peptic ulcers, esophageal varices, and gastritis. Peptic ulcers cause dark, tarry stools due to blood digestion as it passes through the GI tract. Esophageal varices rupture can lead to significant melaena, indicating severe portal hypertension complications.
Peptic Ulcer Disease as a Source of Melaena
Peptic Ulcer Disease (PUD) is a common cause of melaena due to the erosion of the gastric or duodenal mucosa leading to bleeding in the upper gastrointestinal tract. Blood from a bleeding peptic ulcer mixes with gastric secretions and undergoes enzymatic digestion, resulting in the characteristic black, tarry stools of melaena. Endoscopic evaluation is essential for diagnosing the source of bleeding and guiding appropriate treatment to prevent complications such as anemia or perforation.
Esophageal Varices and Melaena Presentation
Esophageal varices, dilated submucosal veins in the lower esophagus, often rupture in patients with portal hypertension, causing upper gastrointestinal bleeding that presents as melaena. Melaena is characterized by black, tarry stools resulting from the digestion of blood as it passes through the GI tract. Early recognition of melaena in patients with esophageal varices is critical for prompt endoscopic intervention and management to prevent severe hemorrhage and maintain hemodynamic stability.
Gastric Cancer Leading to Melaena: Case Insights
Gastric cancer often causes melaena due to tumor-induced ulceration and bleeding within the gastrointestinal tract. In advanced stages, the tumor erodes gastric blood vessels, resulting in black, tarry stools characteristic of upper GI bleeding. Early detection and treatment of gastric malignancies can reduce the severity and frequency of melaena episodes.
Melaena from Mallory-Weiss Tears: Real Patient Scenarios
Melaena from Mallory-Weiss tears presents as dark, tarry stools due to upper gastrointestinal bleeding caused by mucosal lacerations at the gastroesophageal junction. Patients often report episodes of forceful vomiting leading to these linear tears, with bleeding varying from minor to severe, sometimes requiring endoscopic intervention. Real patient scenarios highlight that early diagnosis through endoscopy and prompt management with hemostatic techniques or proton pump inhibitors significantly reduce morbidity associated with this condition.
Rare Causes of Melaena in the GI Tract
Rare causes of melaena in the gastrointestinal tract include vascular lesions such as angiodysplasia and Dieulafoy's lesion, which often present with obscure bleeding. Other uncommon etiologies involve small bowel tumors, such as gastrointestinal stromal tumors (GISTs) and neuroendocrine tumors, which can lead to occult blood loss. Rare infections like intestinal tuberculosis and parasitic infestations may also result in melaena, particularly in endemic regions.
Diagnostic Approach to Melaena in GI Bleeding
Melaena presents as black, tarry stools indicating upper gastrointestinal bleeding often originating from sources such as peptic ulcers, gastric erosions, or esophageal varices. Diagnostic approach includes endoscopy as the gold standard for localization and treatment, supported by complete blood count, coagulation profile, and nasogastric lavage to assess ongoing bleeding. Imaging modalities like CT angiography or tagged red blood cell scans aid in detecting obscure or active bleeding sites when endoscopy is inconclusive.
Management Strategies for Melaena in Clinical Practice
Melaena, characterized by black, tarry stools indicating upper gastrointestinal bleeding, requires prompt endoscopic evaluation to identify the source and facilitate therapeutic interventions such as band ligation or cauterization. Management strategies prioritize hemodynamic stabilization through intravenous fluids and blood transfusions, paired with proton pump inhibitors to reduce gastric acid secretion and promote clot stability. Close monitoring in a clinical setting is essential to detect rebleeding and guide subsequent interventions, including angiographic embolization or surgery in refractory cases.
example of melaena in GI tract Infographic
 samplerz.com
samplerz.com