Iatrogenesis refers to complications or adverse effects that result directly from medical treatment or intervention. An example of iatrogenesis is a postoperative infection caused by non-sterile surgical instruments during a routine appendectomy. This infection can lead to prolonged hospital stays, increased healthcare costs, and additional treatments, highlighting the significance of strict sterilization protocols. Another common example of iatrogenesis is medication-induced side effects, such as kidney damage from prolonged use of nonsteroidal anti-inflammatory drugs (NSAIDs). These adverse drug reactions often require discontinuation or modification of therapy, emphasizing the importance of careful dosing and monitoring. Understanding iatrogenic complications helps healthcare providers improve patient safety and promote better clinical outcomes.
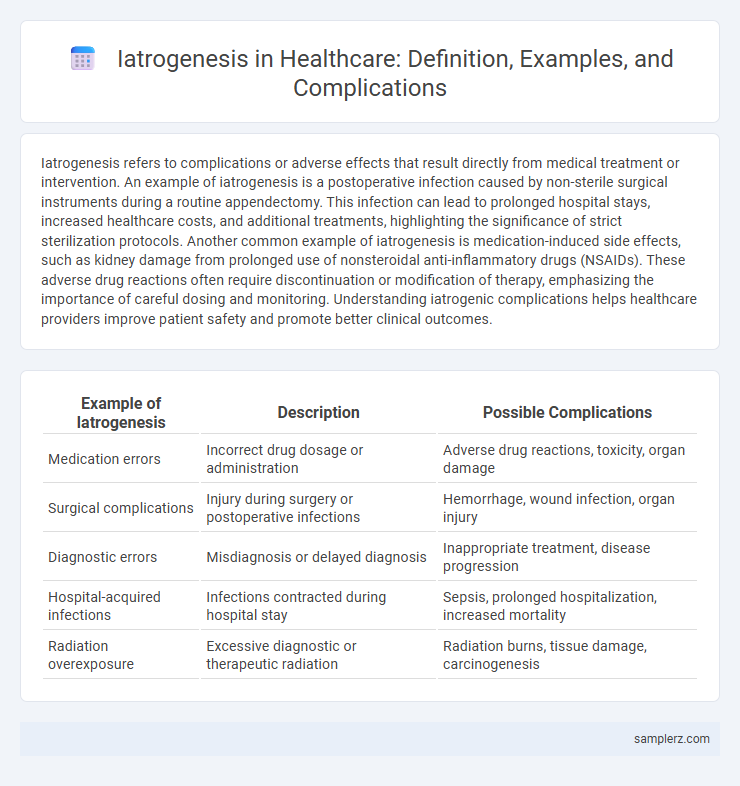
Table of Comparison
| Example of Iatrogenesis | Description | Possible Complications |
|---|---|---|
| Medication errors | Incorrect drug dosage or administration | Adverse drug reactions, toxicity, organ damage |
| Surgical complications | Injury during surgery or postoperative infections | Hemorrhage, wound infection, organ injury |
| Diagnostic errors | Misdiagnosis or delayed diagnosis | Inappropriate treatment, disease progression |
| Hospital-acquired infections | Infections contracted during hospital stay | Sepsis, prolonged hospitalization, increased mortality |
| Radiation overexposure | Excessive diagnostic or therapeutic radiation | Radiation burns, tissue damage, carcinogenesis |
Common Examples of Iatrogenic Complications in Healthcare
Common examples of iatrogenic complications in healthcare include medication errors, such as adverse drug reactions caused by incorrect prescriptions or dosages. Surgical site infections often arise from inadequate sterile techniques during procedures. Other frequent instances involve hospital-acquired infections like catheter-associated urinary tract infections and ventilator-associated pneumonia, which contribute significantly to patient morbidity.
Medication Errors Leading to Iatrogenic Harm
Medication errors represent a significant source of iatrogenic harm, with adverse drug events accounting for a substantial proportion of hospital complications. Incorrect dosing, improper drug selection, and failure to monitor patients can lead to severe outcomes such as organ toxicity, allergic reactions, or therapeutic failure. Implementing electronic prescribing systems and rigorous cross-checking protocols reduces the incidence of medication-related iatrogenesis and improves patient safety.
Surgical Complications Resulting from Iatrogenesis
Surgical complications resulting from iatrogenesis include infections, hemorrhage, and organ damage caused by errors during medical procedures. Iatrogenic injuries often stem from sterile technique breaches, surgical instrument mishandling, or anesthesia complications. Studies show that approximately 10-15% of postoperative complications are iatrogenic, underscoring the necessity for rigorous surgical protocols and clinician training.
Diagnostic Procedures and Associated Iatrogenic Risks
Diagnostic procedures such as biopsies and imaging studies carry inherent iatrogenic risks including infection, bleeding, and radiation exposure. Misinterpretation of diagnostic results can lead to unnecessary treatments that further increase patient morbidity. These complications highlight the critical need for precise technique and careful assessment to minimize iatrogenic harm during diagnostic evaluations.
Hospital-Acquired Infections as Iatrogenic Complications
Hospital-acquired infections (HAIs) represent a significant example of iatrogenic complications, occurring when patients contract infections during medical treatment in healthcare settings. Common HAIs include bloodstream infections, pneumonia, urinary tract infections, and surgical site infections, often caused by multidrug-resistant organisms like MRSA and Clostridium difficile. Preventative measures such as strict hand hygiene, sterilization protocols, and antimicrobial stewardship are critical in reducing the incidence and impact of these iatrogenic infections on patient outcomes.
Iatrogenic Complications from Medical Device Use
Iatrogenic complications from medical device use include infections from catheter insertions, device malfunctions causing tissue damage, and unintended allergic reactions to implant materials. For instance, central venous catheters can introduce bloodstream infections, while pacemaker lead displacement may result in cardiac injury. Monitoring device performance and adherence to sterile protocols are critical to minimizing these risks.
Adverse Drug Reactions Induced by Medical Intervention
Adverse Drug Reactions (ADRs) represent a prominent example of iatrogenesis in healthcare, where medical interventions inadvertently cause harm. Common ADRs include allergic reactions, drug interactions, and toxic side effects resulting from medication errors or inappropriate prescribing. Monitoring pharmacovigilance data and implementing precision medicine protocols are critical strategies to minimize these iatrogenic complications.
Iatrogenic Injuries in Intensive Care Units
Iatrogenic injuries in Intensive Care Units (ICUs) often result from invasive procedures such as central venous catheterization, mechanical ventilation, or administration of high-risk medications, leading to complications like infections, pneumothorax, and drug toxicity. These injuries significantly contribute to increased patient morbidity, prolonged hospital stays, and higher healthcare costs. Rigorous adherence to evidence-based protocols and continuous staff training are critical in minimizing the incidence of iatrogenic harm in critical care settings.
Psychological Impact of Iatrogenic Events on Patients
Iatrogenic events, such as medication errors or surgical complications, can lead to significant psychological distress in patients, including anxiety, depression, and post-traumatic stress disorder (PTSD). The emotional impact often exacerbates physical symptoms, prolonging recovery and reducing overall quality of life. Effective patient communication and psychological support are critical to mitigate these mental health consequences.
Strategies to Prevent Iatrogenic Complications in Clinical Practice
Iatrogenic complications such as medication errors, hospital-acquired infections, and surgical injury significantly impact patient outcomes. Implementing electronic health records (EHR) with clinical decision support systems (CDSS), strict adherence to infection control protocols, and comprehensive staff training are essential strategies to minimize these risks. Regular auditing and feedback mechanisms further enhance patient safety by identifying and addressing potential sources of iatrogenesis in clinical settings.
example of iatrogenesis in complication Infographic
 samplerz.com
samplerz.com