Prosopagnosia, also known as face blindness, is a neurological condition characterized by the inability to recognize familiar faces. It often results from damage to the fusiform gyrus, a brain area critical for facial recognition. Patients with prosopagnosia may fail to identify close family members or friends, relying instead on non-facial cues like voice or clothing. In neurology, prosopagnosia can be acquired after brain injury, stroke, or neurodegenerative diseases affecting the temporal lobe. Developmental prosopagnosia occurs without brain damage, presenting from early childhood with normal intellectual function. Diagnostic tools include neuroimaging and behavioral face recognition tests to assess the severity and impact on social interactions.
Table of Comparison
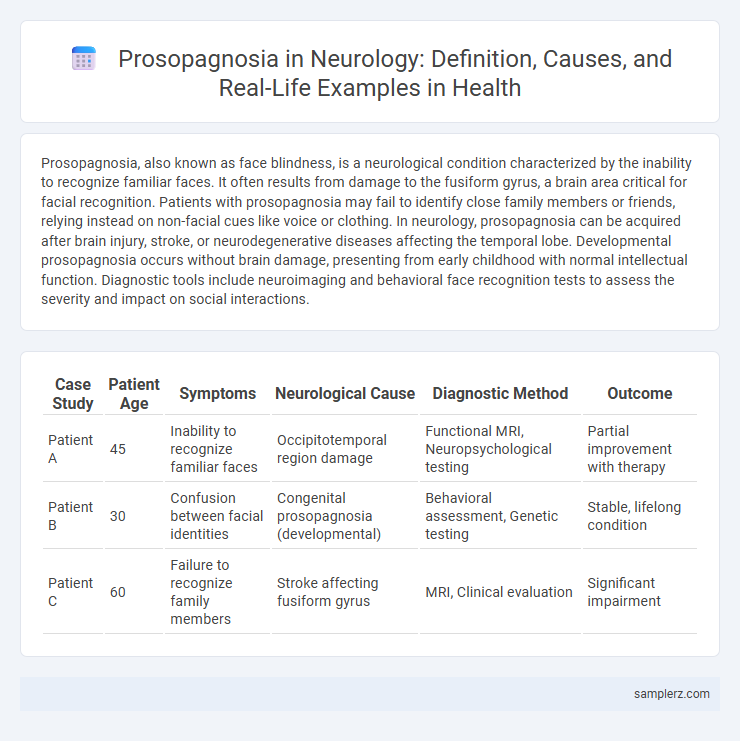
| Case Study | Patient Age | Symptoms | Neurological Cause | Diagnostic Method | Outcome |
|---|---|---|---|---|---|
| Patient A | 45 | Inability to recognize familiar faces | Occipitotemporal region damage | Functional MRI, Neuropsychological testing | Partial improvement with therapy |
| Patient B | 30 | Confusion between facial identities | Congenital prosopagnosia (developmental) | Behavioral assessment, Genetic testing | Stable, lifelong condition |
| Patient C | 60 | Failure to recognize family members | Stroke affecting fusiform gyrus | MRI, Clinical evaluation | Significant impairment |
Understanding Prosopagnosia: Definition and Overview
Prosopagnosia, also known as face blindness, is a neurological disorder characterized by the inability to recognize familiar faces, including those of close family members. This condition often results from damage to the fusiform gyrus, a critical brain region involved in facial recognition, typically due to stroke, traumatic brain injury, or neurodegenerative diseases. Understanding prosopagnosia involves exploring its cognitive mechanisms and impact on social interactions, highlighting the importance of early diagnosis and tailored rehabilitation strategies in neurology.
Neurological Basis of Prosopagnosia
Prosopagnosia, also known as face blindness, results from damage to the fusiform gyrus located in the inferior temporal lobe, which is crucial for facial recognition. Functional MRI studies reveal reduced activity in the fusiform face area (FFA) in individuals with this condition, indicating impaired neural processing of facial features. This neurological basis underscores the role of specialized brain circuits in recognizing and differentiating human faces.
Recognizing Symptoms of Face Blindness
Prosopagnosia, or face blindness, manifests as difficulty recognizing familiar faces, including close family members and oneself in a mirror. Common symptoms include confusion when identifying people, reliance on non-facial cues such as voice or clothing, and avoidance of social situations due to embarrassment. Neurological assessments often reveal impairments in the fusiform gyrus, a brain region crucial for facial recognition.
Case Study: Real-life Example of Prosopagnosia
A well-documented case study of prosopagnosia involves patient B.W., who experienced severe face recognition deficits following bilateral occipitotemporal lesions. Neuroimaging revealed damage to the fusiform face area (FFA), confirming its crucial role in facial processing. Despite intact vision and cognitive functions, B.W. could not recognize familiar faces, demonstrating the specificity of prosopagnosia in neurology.
How Prosopagnosia Impacts Daily Life
Prosopagnosia, also known as face blindness, impairs the brain's ability to recognize familiar faces, significantly affecting social interactions and daily communication. Individuals with prosopagnosia often rely on alternative cues such as voice, clothing, or distinctive features to identify people, which can lead to social anxiety and isolation. The condition challenges routines like greeting colleagues, recognizing family members, or navigating social events, impacting emotional well-being and interpersonal relationships.
Diagnostic Techniques in Neurology for Prosopagnosia
Diagnostic techniques for prosopagnosia in neurology primarily include functional magnetic resonance imaging (fMRI), which identifies abnormalities in the fusiform face area essential for facial recognition. Neuropsychological assessments such as the Cambridge Face Memory Test provide quantitative measures of impairment severity. Electroencephalography (EEG) and event-related potentials (ERPs) further assist in evaluating neural processing delays or deficits linked to face perception anomalies.
Distinguishing Prosopagnosia from Other Visual Disorders
Prosopagnosia, characterized by the inability to recognize familiar faces, is distinct from other visual disorders such as visual agnosia or general memory impairments. Unlike general visual deficits, prosopagnosia specifically affects facial recognition despite intact visual acuity and cognitive function. Neurological assessments often utilize facial recognition tests to differentiate prosopagnosia from disorders involving object recognition or broader visual processing impairments.
Treatment and Management Strategies
Prosopagnosia, a neurological disorder characterized by the inability to recognize faces, lacks a definitive cure but can be managed through compensatory strategies such as training patients to use alternative cues like voice, clothing, or distinctive features for identification. Cognitive rehabilitation techniques and the use of assistive technology, including facial recognition apps, are effective in enhancing daily functioning and social interactions. Ongoing support from neurologists, psychologists, and occupational therapists plays a critical role in developing personalized management plans tailored to the severity and specific challenges of each patient.
Living with Prosopagnosia: Patient Perspectives
Living with prosopagnosia presents daily challenges as patients struggle to recognize familiar faces, impacting social interactions and personal relationships. Neurological studies highlight that individuals often rely on alternative cues such as voice, clothing, or context to identify others, adapting coping strategies over time. Patient perspectives reveal the emotional toll and the importance of support systems to improve quality of life for those with face blindness.
Advances in Neurological Research on Face Blindness
Recent advances in neurological research on prosopagnosia, or face blindness, have identified specific brain regions such as the fusiform face area (FFA) that are critical for facial recognition. Neuroimaging techniques like functional MRI have revealed altered activation patterns in individuals with prosopagnosia, enhancing diagnostic precision and guiding targeted therapies. Genetic studies and neuroplasticity research offer promising avenues for developing rehabilitative interventions to improve facial recognition skills.
example of prosopagnosia in neurology Infographic
 samplerz.com
samplerz.com