Anosmia, the loss of the sense of smell, is a common symptom observed in COVID-19 patients. This condition is often one of the earliest indicators of SARS-CoV-2 infection, occurring even in the absence of other respiratory symptoms. Studies have shown that anosmia affects approximately 40-60% of individuals infected with the virus, making it a significant clinical feature for early diagnosis. The underlying mechanism involves the virus targeting the olfactory epithelium in the nasal cavity, leading to inflammation and disruption of sensory neuron function. Data from various health organizations confirm that anosmia related to COVID-19 can persist for weeks or months in some cases, impacting patients' quality of life. Monitoring this symptom has become vital in controlling the spread of the virus and providing timely medical intervention.
Table of Comparison
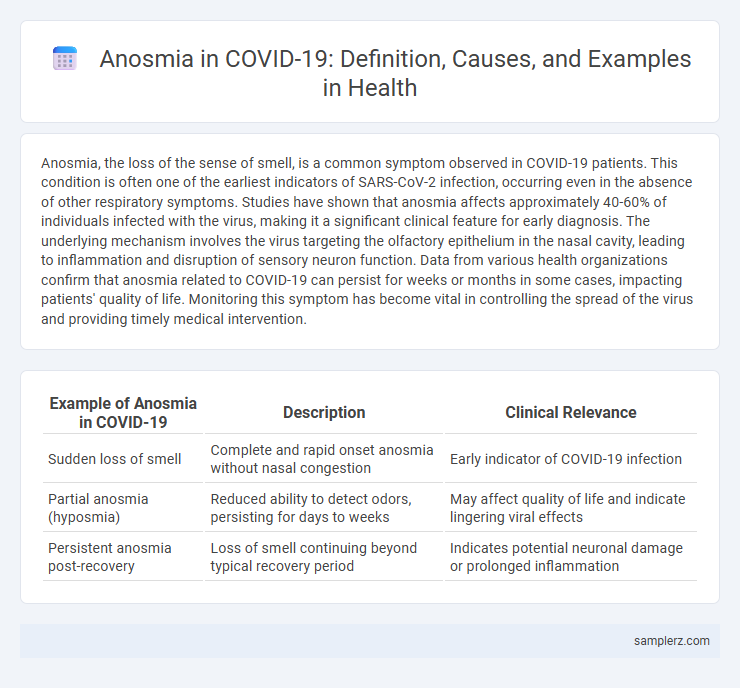
| Example of Anosmia in COVID-19 | Description | Clinical Relevance |
|---|---|---|
| Sudden loss of smell | Complete and rapid onset anosmia without nasal congestion | Early indicator of COVID-19 infection |
| Partial anosmia (hyposmia) | Reduced ability to detect odors, persisting for days to weeks | May affect quality of life and indicate lingering viral effects |
| Persistent anosmia post-recovery | Loss of smell continuing beyond typical recovery period | Indicates potential neuronal damage or prolonged inflammation |
Introduction to Anosmia in COVID-19
Anosmia, the loss of the sense of smell, has emerged as a key symptom in COVID-19 patients, often occurring early in the infection. Studies indicate that SARS-CoV-2 targets olfactory receptor neurons and supporting cells in the nasal epithelium, disrupting normal olfactory function. Recognizing anosmia as a diagnostic marker aids in early detection and isolation, helping to reduce virus transmission.
Early Reports of Smell Loss in COVID-19 Patients
Early reports of anosmia in COVID-19 patients identified smell loss as a significant symptom even in mild cases, with studies from March 2020 noting up to 60% of infected individuals experiencing olfactory dysfunction. Research published in journals like The Laryngoscope highlighted sudden onset anosmia as a key diagnostic indicator, often preceding other symptoms such as fever and cough. These findings emphasized the importance of recognizing qualitative and quantitative smell changes for early detection and isolation of SARS-CoV-2 infections.
Case Study: Sudden Anosmia Without Nasal Congestion
A notable case study of sudden anosmia in COVID-19 involves a 35-year-old patient who experienced complete loss of smell without any nasal congestion or rhinorrhea, highlighting anosmia as an isolated symptom. Diagnostic RT-PCR confirmed SARS-CoV-2 infection, and olfactory testing demonstrated severe hyposmia within days of symptom onset. This case underscores the importance of recognizing sudden anosmia as a potential early indicator of COVID-19, even in the absence of typical nasal symptoms.
Severity of Anosmia in Mild vs Severe COVID-19 Cases
Anosmia, the loss of smell, is a prevalent symptom in COVID-19 and varies significantly in severity between mild and severe cases. Mild COVID-19 patients often experience transient and partial anosmia, while severe cases may present prolonged or complete loss of olfactory function due to extensive viral damage in the olfactory epithelium and central nervous system involvement. Studies indicate that anosmia severity correlates with viral load and immune response intensity, highlighting its potential as a clinical marker for disease progression.
Duration and Recovery Patterns of COVID-19-related Anosmia
COVID-19-related anosmia typically lasts from two weeks to two months, with most patients experiencing significant recovery within the first four weeks. Recovery patterns vary, with some individuals reporting partial return of smell within days, while others experience prolonged or fluctuating olfactory dysfunction lasting several months. Studies show that early intervention and olfactory training can improve outcomes and speed up recovery in persistent cases.
Anosmia as a Diagnostic Symptom for COVID-19
Anosmia, the sudden loss of smell, has emerged as a significant diagnostic symptom of COVID-19, frequently preceding other clinical manifestations. Studies indicate that up to 60% of COVID-19 patients experience anosmia, making it a valuable early indicator for SARS-CoV-2 infection. Incorporating anosmia into screening protocols improves early detection rates and aids in timely quarantine measures to curb virus transmission.
Anosmia in Asymptomatic or Pauci-symptomatic COVID-19 Patients
Anosmia frequently occurs in asymptomatic or pauci-symptomatic COVID-19 patients, serving as an early indicator of SARS-CoV-2 infection. Studies reveal that up to 60% of mild or asymptomatic cases experience sudden loss of smell without other overt symptoms. The presence of anosmia in these patients aids in early detection and isolation, helping to control virus transmission.
Comparison of Anosmia in COVID-19 and Other Viral Infections
Anosmia, or loss of smell, is a distinctive symptom observed in COVID-19, occurring in approximately 40-60% of patients, which is significantly higher compared to other viral infections like influenza or the common cold, where anosmia prevalence is typically below 20%. The mechanism in COVID-19 involves direct viral damage to the olfactory epithelium and nearby support cells, differing from other viruses that primarily cause nasal congestion leading to temporary smell loss. Recovery of smell in COVID-19 cases varies from weeks to months, whereas anosmia from other viral infections often resolves more rapidly following resolution of nasal inflammation.
Impact of Anosmia on Quality of Life During COVID-19 Infection
Anosmia, a common symptom of COVID-19, significantly impairs patients' quality of life by disrupting the ability to detect odors, which affects taste, appetite, and nutrition. The loss of smell can lead to emotional distress, social isolation, and safety risks such as inability to detect smoke or gas leaks. Studies indicate that prolonged anosmia correlates with increased anxiety and depression among COVID-19 survivors, highlighting the need for targeted therapeutic interventions.
Management and Treatment Options for COVID-19-induced Anosmia
Management of COVID-19-induced anosmia primarily involves olfactory training, which includes repeated exposure to a set of odorants to stimulate olfactory nerve regeneration. Corticosteroids, both systemic and intranasal, are sometimes prescribed to reduce inflammation in the olfactory cleft, although their efficacy varies among patients. Emerging treatments such as platelet-rich plasma (PRP) injections and vitamin A supplementation are being investigated for their potential to enhance olfactory recovery in persistent cases.
example of anosmia in COVID-19 Infographic
 samplerz.com
samplerz.com