Melanosis in dermatology refers to an abnormal increase of melanin or pigmentation in the skin. An example of melanosis is lentigo, which presents as well-demarcated, flat, brown to black spots on sun-exposed areas. This condition is commonly linked to chronic sun exposure and aging, reflecting localized melanocyte activity. Another example is oral melanosis, which manifests as dark pigmentation on the mucous membranes inside the mouth. Oral melanosis often occurs due to smoking or certain medications, leading to increased melanin production in the oral epithelium. Clinicians use biopsy and dermoscopy to differentiate melanosis from malignant lesions, ensuring accurate diagnosis and treatment.
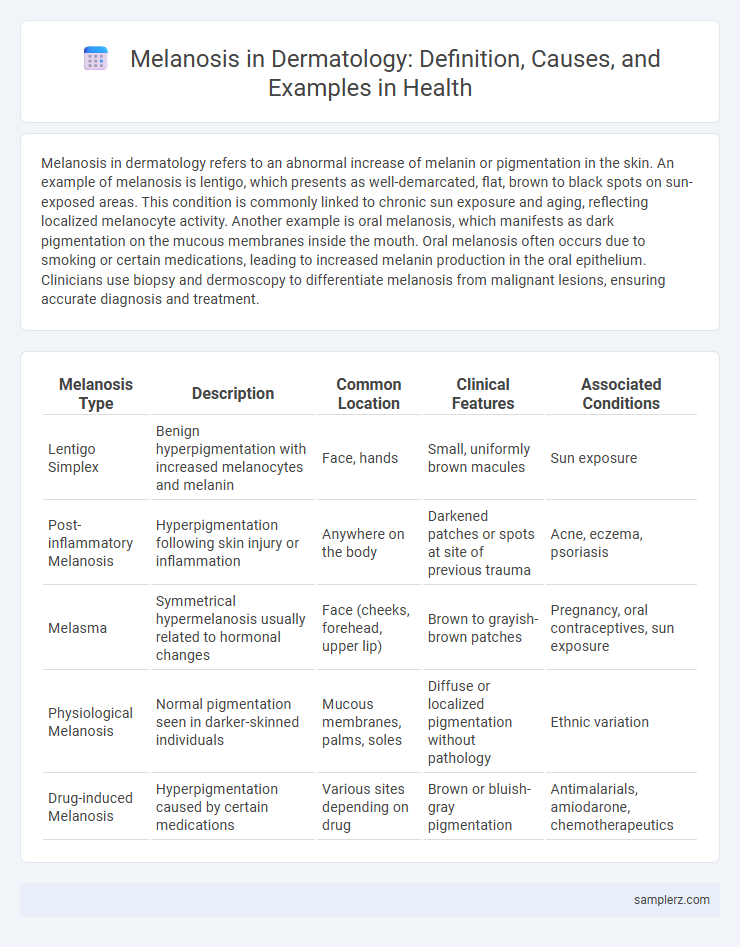
Table of Comparison
| Melanosis Type | Description | Common Location | Clinical Features | Associated Conditions |
|---|---|---|---|---|
| Lentigo Simplex | Benign hyperpigmentation with increased melanocytes and melanin | Face, hands | Small, uniformly brown macules | Sun exposure |
| Post-inflammatory Melanosis | Hyperpigmentation following skin injury or inflammation | Anywhere on the body | Darkened patches or spots at site of previous trauma | Acne, eczema, psoriasis |
| Melasma | Symmetrical hypermelanosis usually related to hormonal changes | Face (cheeks, forehead, upper lip) | Brown to grayish-brown patches | Pregnancy, oral contraceptives, sun exposure |
| Physiological Melanosis | Normal pigmentation seen in darker-skinned individuals | Mucous membranes, palms, soles | Diffuse or localized pigmentation without pathology | Ethnic variation |
| Drug-induced Melanosis | Hyperpigmentation caused by certain medications | Various sites depending on drug | Brown or bluish-gray pigmentation | Antimalarials, amiodarone, chemotherapeutics |
Understanding Melanosis: Definition and Overview
Melanosis in dermatology refers to abnormal dark pigmentation caused by an excess deposition of melanin in the skin. This condition can present as localized or widespread hyperpigmented macules or patches, often linked to conditions such as melanosis coli, post-inflammatory hyperpigmentation, or drug-induced melanosis. Identifying the underlying cause involves clinical examination, histopathological analysis, and evaluation of patient history to differentiate benign melanosis from malignant melanocytic lesions.
Common Types of Melanosis in Dermatology
Common types of melanosis in dermatology include melanosis coli, characterized by brownish pigmentation of the colonic mucosa often linked to chronic laxative use, and physiologic melanosis, which presents as benign hyperpigmentation in areas like the palms and soles. Other notable examples are drug-induced melanosis caused by medications such as minocycline or antimalarials, and post-inflammatory melanosis resulting from skin injuries or inflammatory conditions like eczema and psoriasis. Recognition of these types is crucial for accurate diagnosis and management of hyperpigmented lesions in clinical practice.
Clinical Features of Cutaneous Melanosis
Cutaneous melanosis presents as hyperpigmented patches or macules with varying shades of brown to black, often localized or diffuse on the skin. These lesions may exhibit irregular borders and are usually asymptomatic but can be associated with conditions like post-inflammatory hyperpigmentation or lentigo simplex. Dermoscopic examination often reveals homogeneous pigmentation patterns, aiding in differentiation from malignant melanocytic lesions.
Oral Melanosis: Causes and Presentation
Oral melanosis manifests as dark brown or black pigmentation on the mucous membranes of the oral cavity, commonly linked to chronic tobacco use, certain medications, or systemic conditions like Addison's disease. Melanotic macules and smoker's melanosis are frequent presentations, characterized by flat, asymptomatic, pigmented patches primarily on the buccal mucosa or gingiva. Diagnosis involves clinical examination and, if necessary, biopsy to distinguish benign melanosis from malignant melanocytic lesions such as oral melanoma.
Drug-Induced Melanosis: Examples and Mechanisms
Drug-induced melanosis in dermatology manifests as hyperpigmentation caused by certain medications, such as antimalarials, minocycline, and amiodarone. These drugs induce melanosis through mechanisms involving increased melanin production, deposition of the drug or its metabolites in the skin, and stimulation of melanocyte activity. Recognizing drug-induced melanosis is crucial for differentiating it from other pigmented lesions and managing drug-related side effects effectively.
Melanosis Associated with Systemic Diseases
Melanosis associated with systemic diseases commonly presents as hyperpigmentation linked to underlying disorders such as Addison's disease, hemochromatosis, and chronic liver disease. In Addison's disease, increased melanocyte-stimulating hormone results in diffuse, patchy pigmentation, especially in sun-exposed areas and mucous membranes. Hemochromatosis causes bronze discoloration due to iron deposition, while chronic liver disease leads to melanin accumulation, contributing to generalized skin darkening.
Diagnostic Techniques for Identifying Melanosis
Dermatoscopy is a key diagnostic technique for identifying melanosis, allowing detailed visualization of pigment patterns and vascular structures on the skin surface. Reflectance confocal microscopy provides non-invasive, high-resolution imaging that helps distinguish benign melanosis from malignant lesions. Histopathological examination remains the gold standard for confirming melanosis diagnosis by analyzing melanocyte proliferation and melanin distribution in skin biopsies.
Melanosis Nigricans: Distinguishing Features
Melanosis Nigricans is characterized by hyperpigmented, velvety plaques commonly found in intertriginous areas like the neck, axillae, and groin. It often associates with insulin resistance, obesity, or endocrinopathies, serving as a cutaneous marker for these systemic conditions. Histopathology reveals increased basal layer melanin and papillomatosis without melanocytic proliferation, aiding differential diagnosis from malignant melanoma.
Management and Treatment of Melanosis
Management of melanosis in dermatology primarily involves identifying and eliminating the underlying cause, such as exposure to certain chemicals or medications. Treatment options include topical depigmenting agents like hydroquinone, retinoids, and corticosteroids to reduce pigmentation. Laser therapy and chemical peels may be recommended for persistent or cosmetically concerning lesions, while regular monitoring ensures early detection of any malignant transformation.
Prognosis and Long-Term Implications of Melanosis
Melanosis, characterized by abnormal melanin accumulation in the skin, generally presents a benign prognosis when identified early and properly managed. Persistent melanosis may lead to cosmetic concerns and occasional dyschromia but rarely progresses to malignant melanoma. Long-term implications include the need for regular dermatologic monitoring to detect any atypical changes indicative of malignant transformation, especially in patients with extensive sun exposure or genetic predisposition.
example of melanosis in dermatology Infographic
 samplerz.com
samplerz.com