Polypharmacy in geriatrics often involves the concurrent use of multiple medications, such as antihypertensives, anticoagulants, and antidiabetic agents, to manage chronic conditions in elderly patients. This practice increases the risk of adverse drug interactions and side effects due to altered pharmacokinetics and pharmacodynamics in aging bodies. Common examples include an elderly patient prescribed metformin for diabetes, lisinopril for hypertension, and aspirin for cardiovascular protection. Healthcare providers monitor patients closely to prevent complications like drug toxicity and cognitive impairment linked to polypharmacy. Data shows that over 40% of elderly patients in clinical settings take five or more medications daily, raising safety concerns. Effective management strategies include regular medication reviews and deprescribing unnecessary drugs to improve outcomes in geriatric care.
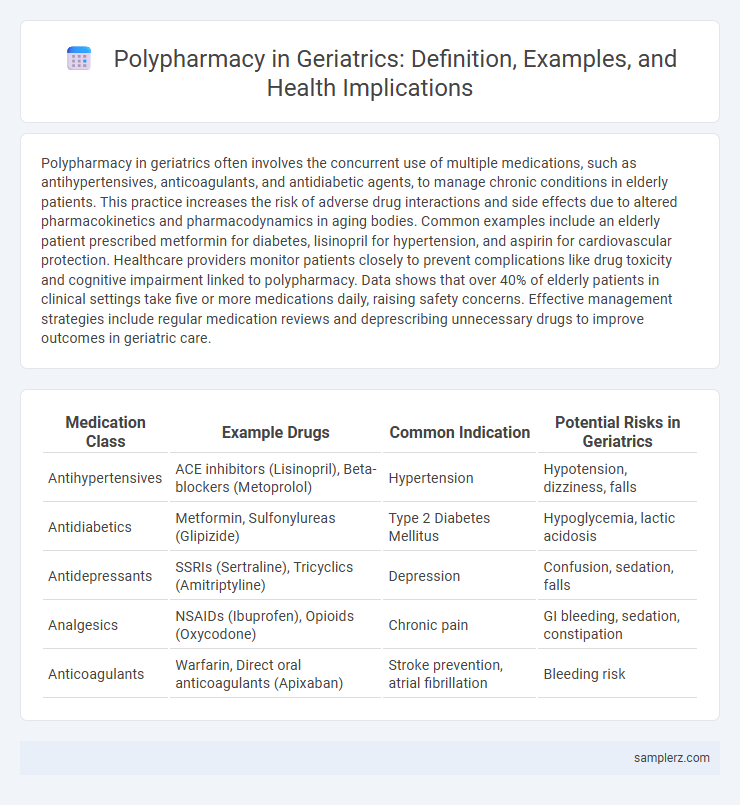
Table of Comparison
| Medication Class | Example Drugs | Common Indication | Potential Risks in Geriatrics |
|---|---|---|---|
| Antihypertensives | ACE inhibitors (Lisinopril), Beta-blockers (Metoprolol) | Hypertension | Hypotension, dizziness, falls |
| Antidiabetics | Metformin, Sulfonylureas (Glipizide) | Type 2 Diabetes Mellitus | Hypoglycemia, lactic acidosis |
| Antidepressants | SSRIs (Sertraline), Tricyclics (Amitriptyline) | Depression | Confusion, sedation, falls |
| Analgesics | NSAIDs (Ibuprofen), Opioids (Oxycodone) | Chronic pain | GI bleeding, sedation, constipation |
| Anticoagulants | Warfarin, Direct oral anticoagulants (Apixaban) | Stroke prevention, atrial fibrillation | Bleeding risk |
Understanding Polypharmacy in Geriatric Patients
Polypharmacy in geriatric patients often involves the simultaneous use of multiple medications such as antihypertensives, antidiabetics, and anticoagulants to manage chronic conditions like hypertension, diabetes, and atrial fibrillation. This complex medication regimen increases the risk of adverse drug reactions, drug-drug interactions, and challenges in adherence due to cognitive decline or physical limitations common in elderly populations. Recognizing the patterns of polypharmacy is crucial for optimizing treatment outcomes and minimizing potential harm in geriatric care.
Common Medications Contributing to Polypharmacy in Older Adults
Common medications contributing to polypharmacy in older adults include antihypertensives like ACE inhibitors and beta-blockers, statins for cholesterol management, and antidiabetic drugs such as metformin. Pain relievers, including NSAIDs and opioids, and medications for mental health conditions like benzodiazepines and antidepressants are also frequently involved. These drugs often accumulate due to multiple chronic conditions, increasing the risk of drug interactions and adverse effects in geriatric patients.
Case Studies: Real-life Examples of Polypharmacy in Geriatrics
Elderly patients with multiple chronic conditions often face complex medication regimens, such as an 82-year-old with hypertension, diabetes, osteoarthritis, and depression prescribed over ten different drugs including antihypertensives, insulin, NSAIDs, and antidepressants. Case studies reveal that such polypharmacy increases the risk of adverse drug reactions, hospitalizations, and medication non-adherence, highlighting the need for regular medication reviews. Evidence-based approaches in geriatrics emphasize deprescribing and personalized treatment plans to minimize drug interactions and optimize therapeutic outcomes.
Risks and Complications Associated with Polypharmacy in the Elderly
Polypharmacy in geriatrics often involves the concurrent use of five or more medications, increasing the risk of adverse drug reactions, drug-drug interactions, and medication non-adherence. Elderly patients commonly experience complications such as cognitive impairment, falls, hospitalizations, and increased mortality related to inappropriate medication regimens. Careful medication review and management strategies are crucial to minimize these risks and improve health outcomes in the aging population.
Typical Drug Combinations in Geriatric Polypharmacy
Common examples of typical drug combinations in geriatric polypharmacy include antihypertensives such as beta-blockers combined with diuretics, alongside antidiabetic agents like metformin. Elderly patients often receive concurrent prescriptions of anticoagulants, statins for hyperlipidemia, and proton pump inhibitors to manage multiple chronic conditions. These combinations require careful monitoring to avoid adverse drug interactions and ensure optimal therapeutic outcomes.
Identifying Symptoms of Adverse Drug Reactions in Seniors
Polypharmacy in geriatrics often leads to complex adverse drug reactions, with symptoms such as confusion, dizziness, gastrointestinal disturbances, and unusual bruising indicating possible drug toxicity or interactions. Monitoring changes in cognitive function, balance, and organ-specific signs like liver or kidney impairment is crucial for early detection. Regular medication reviews and patient education on symptom reporting help mitigate risks and improve therapeutic outcomes in elderly patients.
Polypharmacy and Chronic Disease Management in Older Patients
Polypharmacy in geriatrics commonly occurs in patients managing multiple chronic diseases such as hypertension, diabetes, and osteoarthritis, leading to complex medication regimens that increase the risk of adverse drug reactions and drug-drug interactions. Effective chronic disease management in older adults requires regular medication reviews and personalized adjustments to minimize polypharmacy-related complications. Optimizing pharmacotherapy in geriatric patients improves treatment adherence and overall health outcomes while reducing hospitalizations linked to polypharmacy.
Strategies to Reduce Polypharmacy in Geriatrics
Strategies to reduce polypharmacy in geriatrics include comprehensive medication reviews, deprescribing unnecessary or harmful drugs, and enhancing communication between healthcare providers and patients. Implementing clinical decision support systems and utilizing geriatric assessment tools can optimize medication regimens and minimize adverse drug reactions. Educating patients and caregivers on medication management promotes adherence and reduces the risk of medication errors.
Role of Healthcare Providers in Managing Polypharmacy
Healthcare providers play a critical role in managing polypharmacy in geriatrics by conducting regular medication reviews to identify potentially inappropriate prescriptions and prevent adverse drug interactions. Pharmacists collaborate with physicians to optimize drug regimens, ensuring dosage adjustments based on renal function and comorbidities common in elderly patients. Utilizing electronic health records and clinical decision support systems enhances medication safety and promotes personalized treatment plans for older adults facing multiple chronic conditions.
Best Practices for Safe Medication Use in Elderly Populations
Polypharmacy in geriatrics often involves the concurrent use of multiple medications such as antihypertensives, anticoagulants, and antidiabetics, increasing the risk of adverse drug reactions and drug-drug interactions. Best practices for safe medication use include regular medication reviews, deprescribing unnecessary drugs, and employing clinical decision support tools to optimize therapy. Implementing patient-centered care with thorough monitoring and education reduces hospitalizations and improves treatment outcomes in elderly populations.
example of polypharmacy in geriatrics Infographic
 samplerz.com
samplerz.com