Orthostatic hypotension is a condition characterized by a significant drop in blood pressure when a person stands up from a sitting or lying position. It occurs due to the body's inability to quickly adjust blood vessel constriction and heart rate, leading to reduced blood flow to the brain. Common symptoms include dizziness, lightheadedness, and fainting upon standing. An example of orthostatic hypotension occurs in elderly patients who experience sudden dizziness after rising from bed in the morning. Another instance can be found in individuals taking medications such as diuretics or beta-blockers, which can impair blood pressure regulation. Measuring blood pressure in different positions helps diagnose this condition and guide appropriate treatment.
Table of Comparison
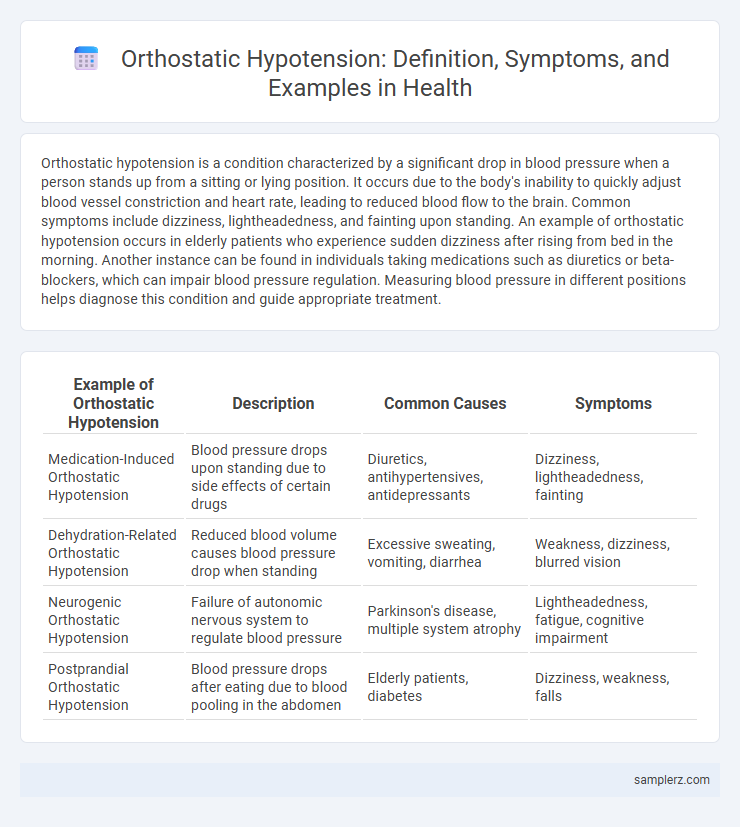
| Example of Orthostatic Hypotension | Description | Common Causes | Symptoms |
|---|---|---|---|
| Medication-Induced Orthostatic Hypotension | Blood pressure drops upon standing due to side effects of certain drugs | Diuretics, antihypertensives, antidepressants | Dizziness, lightheadedness, fainting |
| Dehydration-Related Orthostatic Hypotension | Reduced blood volume causes blood pressure drop when standing | Excessive sweating, vomiting, diarrhea | Weakness, dizziness, blurred vision |
| Neurogenic Orthostatic Hypotension | Failure of autonomic nervous system to regulate blood pressure | Parkinson's disease, multiple system atrophy | Lightheadedness, fatigue, cognitive impairment |
| Postprandial Orthostatic Hypotension | Blood pressure drops after eating due to blood pooling in the abdomen | Elderly patients, diabetes | Dizziness, weakness, falls |
Understanding Orthostatic Hypotension: Key Concepts
Orthostatic hypotension occurs when blood pressure drops significantly upon standing, leading to symptoms like dizziness or fainting. This condition results from inadequate autonomic nervous system response, causing insufficient blood flow to the brain. Monitoring systolic blood pressure changes of at least 20 mmHg or diastolic drops of 10 mmHg within three minutes of standing helps diagnose the disorder effectively.
Common Causes of Orthostatic Hypotension
Orthostatic hypotension commonly results from dehydration, which reduces blood volume and impairs vascular regulation. Other frequent causes include medications like diuretics and antihypertensives, as well as autonomic nervous system disorders such as Parkinson's disease. Elderly individuals often experience this condition due to impaired baroreceptor sensitivity and prolonged bed rest.
Recognizing Symptoms of Postural Low Blood Pressure
Recognizing symptoms of orthostatic hypotension involves noting dizziness, lightheadedness, and blurred vision upon standing due to a sudden drop in blood pressure. These signs indicate the body's impaired ability to adjust blood flow when changing posture, leading to reduced cerebral perfusion. Timely identification of postural low blood pressure symptoms is crucial for preventing falls and managing underlying cardiovascular or neurological conditions effectively.
Diagnosing Orthostatic Hypotension: Clinical Criteria
Diagnosing orthostatic hypotension involves measuring blood pressure changes from lying to standing, with a reduction of at least 20 mm Hg systolic or 10 mm Hg diastolic within three minutes indicating the condition. Clinical evaluation includes assessing symptoms such as dizziness, lightheadedness, or syncope upon standing, which correlate with the measurable blood pressure drop. Confirmatory tests may involve tilt table testing and autonomic function assessments to differentiate between neurogenic and non-neurogenic orthostatic hypotension.
Real-Life Examples of Orthostatic Hypotension Episodes
Orthostatic hypotension commonly occurs in elderly patients who experience dizziness or fainting upon standing rapidly from a seated position, often leading to falls. Individuals with diabetes frequently encounter this condition due to autonomic neuropathy affecting blood pressure regulation during posture changes. Athletes dehydrated after intense exercise may also exhibit orthostatic hypotension symptoms like lightheadedness when moving from lying down to standing.
Risk Factors Associated with Orthostatic Hypotension
Risk factors associated with orthostatic hypotension include advanced age, dehydration, and the use of antihypertensive medications such as diuretics and beta-blockers. Neurological disorders like Parkinson's disease and diabetes-induced autonomic neuropathy significantly increase susceptibility to this condition. Identifying these factors aids in early diagnosis and targeted management to prevent falls and related complications.
Complications Arising from Orthostatic Hypotension
Orthostatic hypotension can lead to serious complications such as falls, syncope, and cognitive impairment due to reduced cerebral perfusion. Patients with this condition are at increased risk for fractures and traumatic injuries, often resulting in prolonged hospital stays. Chronic orthostatic hypotension may also exacerbate underlying cardiovascular diseases, further compromising patient health.
Management Strategies for Orthostatic Hypotension
Management strategies for orthostatic hypotension emphasize gradual position changes to prevent dizziness and falls, ensuring patient safety. Hydration optimization and increased salt intake are often recommended to maintain blood volume and improve vascular tone. Pharmacological treatments such as fludrocortisone or midodrine may be prescribed to enhance blood pressure stability in severe cases.
Preventive Measures for Orthostatic Hypotension
Preventive measures for orthostatic hypotension include rising slowly from sitting or lying positions to avoid sudden blood pressure drops. Increasing fluid and salt intake, under medical supervision, helps maintain blood volume and reduces symptoms. Regular physical activity strengthens cardiovascular function, while wearing compression stockings improves venous return and prevents blood pooling in the lower limbs.
Patient Stories: Living with Orthostatic Hypotension
Patients with orthostatic hypotension often describe sudden dizziness and fainting upon standing, severely impacting daily activities. One patient shared how adjusting to slow positional changes and increased hydration reduced symptom severity and improved quality of life. Consistent monitoring and personalized treatment plans remain critical for managing the unpredictable nature of this condition.
example of orthostatic in hypotension Infographic
 samplerz.com
samplerz.com