Hyperalgesia is a condition characterized by an increased sensitivity to pain, often caused by damage to nociceptors or peripheral nerves. For example, patients with diabetic neuropathy frequently experience hyperalgesia, where even mild stimuli, such as light touch or temperature changes, result in intense pain. This heightened pain response occurs due to altered pain signaling pathways within the nervous system. In clinical settings, hyperalgesia is commonly observed after surgery, especially in cases involving nerve injury or inflammation. Post-surgical patients may report severe pain at the incision site that exceeds the expected level based on the wound's appearance. Studies show that hyperalgesia can complicate pain management strategies, requiring tailored analgesic treatments to effectively reduce patient discomfort.
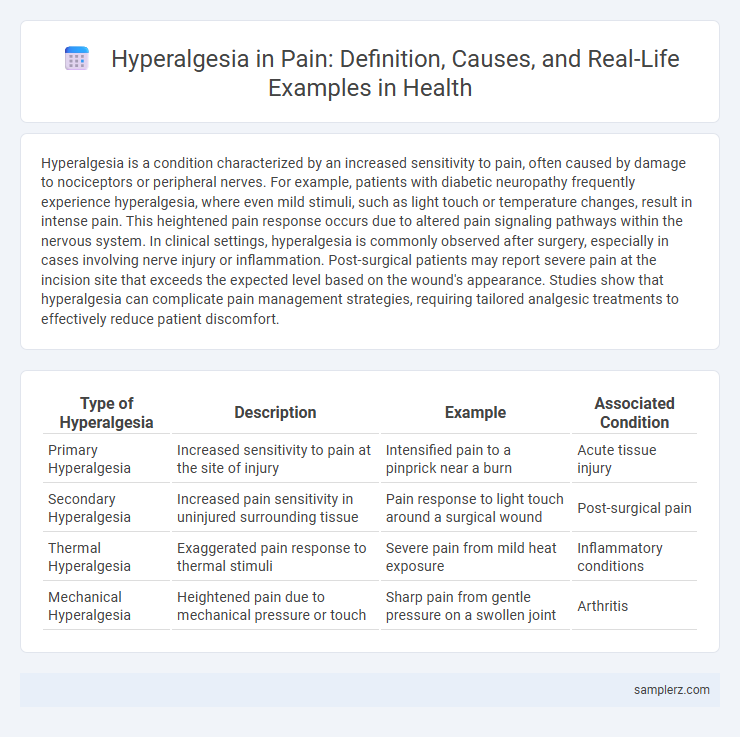
Table of Comparison
| Type of Hyperalgesia | Description | Example | Associated Condition |
|---|---|---|---|
| Primary Hyperalgesia | Increased sensitivity to pain at the site of injury | Intensified pain to a pinprick near a burn | Acute tissue injury |
| Secondary Hyperalgesia | Increased pain sensitivity in uninjured surrounding tissue | Pain response to light touch around a surgical wound | Post-surgical pain |
| Thermal Hyperalgesia | Exaggerated pain response to thermal stimuli | Severe pain from mild heat exposure | Inflammatory conditions |
| Mechanical Hyperalgesia | Heightened pain due to mechanical pressure or touch | Sharp pain from gentle pressure on a swollen joint | Arthritis |
Common Clinical Examples of Hyperalgesia
Common clinical examples of hyperalgesia include neuropathic pain conditions such as diabetic neuropathy, postherpetic neuralgia, and fibromyalgia, where patients experience increased sensitivity to pain stimuli. Inflammatory diseases like rheumatoid arthritis and osteoarthritis often present hyperalgesia due to sensitization of peripheral nociceptors. Opioid-induced hyperalgesia is another frequent example, characterized by paradoxical heightened pain sensitivity following prolonged opioid use.
Postoperative Hyperalgesia: Case Scenarios
Postoperative hyperalgesia often manifests as an increased sensitivity to pain following surgery, where patients experience amplified pain responses at the surgical site despite standard analgesic treatments. Case scenarios reveal that individuals receiving opioids like remifentanil during surgery may develop hyperalgesia, characterized by heightened pain intensity and reduced efficacy of pain medications postoperatively. Understanding these clinical presentations helps tailor pain management strategies, such as multimodal analgesia or opioid-sparing techniques, to mitigate postoperative hyperalgesia and improve patient outcomes.
Opioid-Induced Hyperalgesia: Real-world Instances
Opioid-Induced Hyperalgesia (OIH) manifests when patients receiving long-term opioid therapy, such as morphine or fentanyl, experience increased sensitivity to pain rather than relief. Real-world cases include postoperative pain patients who report exacerbated discomfort despite escalating opioid doses, highlighting the paradoxical effect of opioid treatment. Clinical studies document OIH's prevalence in cancer pain management, where opioid escalation fails and alternative pain control strategies become necessary.
Neuropathic Pain and Hyperalgesia Manifestations
Neuropathic pain often presents with hyperalgesia, where patients experience an exaggerated response to painful stimuli due to nerve damage or dysfunction. Common manifestations include burning, shooting pain, and increased sensitivity to touch or temperature changes, frequently seen in conditions like diabetic neuropathy and postherpetic neuralgia. Understanding hyperalgesia's role in neuropathic pain aids in accurate diagnosis and tailored treatment strategies.
Hyperalgesia in Chronic Inflammatory Conditions
Hyperalgesia in chronic inflammatory conditions manifests as an amplified response to painful stimuli due to persistent inflammation sensitizing peripheral and central nociceptors. Diseases such as rheumatoid arthritis and inflammatory bowel disease frequently exhibit this heightened pain sensitivity, complicating management and reducing quality of life. Targeting the underlying inflammatory pathways with immunomodulatory therapies can help alleviate hyperalgesia and improve patient outcomes.
Hyperalgesia Associated with Diabetic Neuropathy
Hyperalgesia associated with diabetic neuropathy manifests as an exaggerated pain response to normally painful stimuli, often characterized by burning, tingling, or stabbing sensations in the feet and lower legs. This condition results from nerve damage caused by prolonged hyperglycemia, leading to increased sensitivity of peripheral nociceptors and central nervous system sensitization. Managing hyperalgesic pain in diabetic neuropathy involves multimodal approaches, including glycemic control, pharmacological agents like gabapentin and duloxetine, and lifestyle modifications to prevent further nerve damage.
Chemotherapy-Induced Hyperalgesia: Clinical Evidence
Chemotherapy-induced hyperalgesia manifests as increased pain sensitivity following cancer treatment, particularly with platinum-based drugs and taxanes. Clinical studies reveal patients often experience heightened pain responses, such as burning or stabbing sensations, which can persist long after therapy ends. Neurophysiological assessments confirm altered nociceptive pathways, highlighting the need for targeted pain management strategies in oncology care.
Hyperalgesia in Fibromyalgia Patients
Hyperalgesia in fibromyalgia patients manifests as an increased sensitivity to pain stimuli that are typically not as painful to healthy individuals. Studies reveal that altered central nervous system processing and heightened pain receptor activity contribute to this amplified pain perception. Effective management strategies often include pharmacological treatments like duloxetine or pregabalin, combined with cognitive-behavioral therapy to alleviate pain hypersensitivity.
Hyperalgesia Due to Physical Trauma
Hyperalgesia due to physical trauma occurs when damaged tissues cause an exaggerated pain response, such as intense pain following a minor injury like a sprained ankle or surgical incision. This condition often involves peripheral sensitization, where nociceptors become hyper-responsive to stimuli, resulting in increased pain sensitivity around the injury site. Understanding trauma-induced hyperalgesia is crucial for effective pain management strategies, including targeted use of analgesics and physical therapy.
Hyperalgesia in Autoimmune Disorders
Hyperalgesia in autoimmune disorders, such as rheumatoid arthritis and lupus, manifests as an increased sensitivity to pain due to chronic inflammation and immune system dysregulation. Cytokines like tumor necrosis factor-alpha (TNF-a) and interleukin-1b (IL-1b) play crucial roles in sensitizing nociceptive pathways, exacerbating pain perception. This heightened pain response often complicates disease management and requires targeted therapies addressing both inflammation and neural sensitization.
example of hyperalgesia in pain Infographic
 samplerz.com
samplerz.com