Ascites is a common clinical manifestation in hepatology, particularly associated with liver cirrhosis. It results from the accumulation of fluid in the peritoneal cavity due to portal hypertension and hypoalbuminemia. Data show that patients with advanced cirrhosis often develop ascitic fluid rich in protein and inflammatory cells, which helps distinguish it from other causes of fluid accumulation. Diagnosis of ascites involves paracentesis, where a sample of the peritoneal fluid is analyzed for albumin concentration, cell count, and culture. The serum-ascites albumin gradient (SAAG) is a critical parameter used to differentiate portal hypertension-related ascites from other etiologies. Effective management of ascites in hepatology relies on sodium restriction, diuretics, and in refractory cases, procedures like transjugular intrahepatic portosystemic shunt (TIPS).
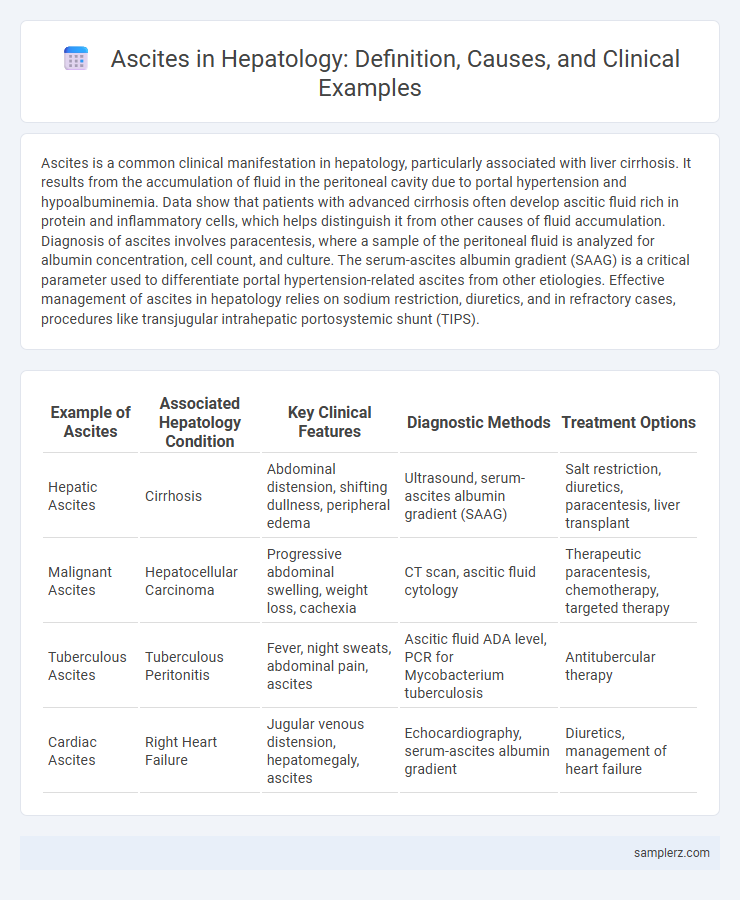
Table of Comparison
| Example of Ascites | Associated Hepatology Condition | Key Clinical Features | Diagnostic Methods | Treatment Options |
|---|---|---|---|---|
| Hepatic Ascites | Cirrhosis | Abdominal distension, shifting dullness, peripheral edema | Ultrasound, serum-ascites albumin gradient (SAAG) | Salt restriction, diuretics, paracentesis, liver transplant |
| Malignant Ascites | Hepatocellular Carcinoma | Progressive abdominal swelling, weight loss, cachexia | CT scan, ascitic fluid cytology | Therapeutic paracentesis, chemotherapy, targeted therapy |
| Tuberculous Ascites | Tuberculous Peritonitis | Fever, night sweats, abdominal pain, ascites | Ascitic fluid ADA level, PCR for Mycobacterium tuberculosis | Antitubercular therapy |
| Cardiac Ascites | Right Heart Failure | Jugular venous distension, hepatomegaly, ascites | Echocardiography, serum-ascites albumin gradient | Diuretics, management of heart failure |
Understanding Ascites: Definition and Pathophysiology
Ascites is the abnormal accumulation of fluid within the peritoneal cavity, commonly resulting from liver cirrhosis and portal hypertension. The pathophysiology involves increased hydrostatic pressure in the portal venous system, hypoalbuminemia reducing plasma oncotic pressure, and sodium retention mediated by renal mechanisms. Understanding these mechanisms is essential for diagnosing and managing ascites in hepatology patients.
Common Causes of Ascites in Hepatology
Ascites in hepatology commonly results from liver cirrhosis, which leads to portal hypertension and impaired albumin synthesis, causing fluid accumulation in the peritoneal cavity. Other prevalent causes include hepatic malignancies such as hepatocellular carcinoma and infections like spontaneous bacterial peritonitis that exacerbate fluid retention. Diagnosing the underlying cause involves analyzing ascitic fluid for parameters like serum-ascites albumin gradient (SAAG) to differentiate portal hypertension-related ascites from other etiologies.
Clinical Presentation: Signs and Symptoms of Ascites
Ascites in hepatology typically presents with abdominal distension, shifting dullness, and fluid wave on physical examination. Patients often experience early satiety, dyspnea due to diaphragmatic elevation, and peripheral edema. Common associated signs include hepatomegaly, jaundice, and variceal bleeding in cirrhotic patients.
Diagnostic Approaches to Ascites in Liver Disease
Diagnostic approaches to ascites in liver disease primarily involve clinical evaluation, imaging studies, and laboratory analysis of ascitic fluid. Ultrasound is the preferred imaging modality to detect fluid accumulation and guide paracentesis, while serum-ascites albumin gradient (SAAG) measurement aids in differentiating portal hypertension-related ascites from other causes. Ascitic fluid analysis includes cell count, protein levels, and culture to diagnose spontaneous bacterial peritonitis, which is a critical complication in cirrhotic patients.
Imaging Techniques for Detecting Ascites
Ultrasound is the primary imaging technique for detecting ascites, offering high sensitivity in identifying even small fluid accumulations within the peritoneal cavity. CT scans provide detailed cross-sectional images that can reveal ascitic fluid distribution and underlying causes such as liver cirrhosis or malignancy. MRI, although less commonly used, offers excellent soft tissue contrast to differentiate ascitic fluid from other abdominal abnormalities, aiding in comprehensive hepatological assessment.
Paracentesis: Procedure and Indications
Paracentesis is a critical procedure in hepatology used to diagnose and relieve ascites, which frequently occurs in liver cirrhosis patients. During paracentesis, a sterile needle is inserted into the peritoneal cavity to remove excess fluid for diagnostic analysis or symptomatic relief. Indications include tense ascites causing respiratory distress or suspected spontaneous bacterial peritonitis requiring fluid culture.
Portal Hypertension and Ascites Formation
Portal hypertension, a common complication of chronic liver disease, leads to increased pressure in the portal venous system, causing fluid to accumulate in the abdominal cavity known as ascites. The elevated portal pressure disrupts normal fluid homeostasis by increasing hydrostatic pressure and impairing lymphatic drainage, while hypoalbuminemia reduces oncotic pressure, collectively promoting ascites formation. Effective management of ascites often requires addressing the underlying portal hypertension through medical therapies or procedures such as transjugular intrahepatic portosystemic shunt (TIPS).
Complications Associated with Ascites in Hepatology
Ascites in hepatology commonly arises from liver cirrhosis and leads to significant complications such as spontaneous bacterial peritonitis, hepatorenal syndrome, and hepatic encephalopathy. The accumulation of ascitic fluid increases intra-abdominal pressure, which can impair renal function and promote bacterial translocation. Management of these complications requires careful monitoring and intervention to prevent morbidity and mortality in patients with advanced liver disease.
Management and Treatment Options for Ascites
Management of ascites in hepatology primarily involves sodium restriction and diuretic therapy, with spironolactone and furosemide being the most commonly used agents. Large-volume paracentesis is indicated for patients with tense ascites, often combined with intravenous albumin to prevent circulatory dysfunction. In refractory cases, transjugular intrahepatic portosystemic shunt (TIPS) placement or liver transplantation may be necessary to control fluid accumulation and improve patient outcomes.
Prognosis and Prevention Strategies for Ascites in Liver Disorders
Ascites in liver disorders, particularly cirrhosis, signals advanced hepatic dysfunction and carries a poor prognosis with increased risk of spontaneous bacterial peritonitis and renal failure. Effective prevention strategies include sodium restriction, judicious use of diuretics like spironolactone and furosemide, and regular monitoring of liver function and ascitic fluid. Early intervention with lifestyle modifications and management of underlying liver disease may improve survival rates and reduce ascites recurrence.
example of ascites in hepatology Infographic
 samplerz.com
samplerz.com