A common example of a nosocomial infection in hospitals is Methicillin-resistant Staphylococcus aureus (MRSA). This bacteria causes severe skin infections and pneumonia and is resistant to many standard antibiotics. MRSA spreads primarily through direct contact with contaminated surfaces or healthcare personnel. Clostridium difficile infection (CDI) is another prevalent nosocomial infection. It leads to severe diarrhea and colitis after antibiotic use disrupts normal gut flora. Hospitals often report CDI cases linked to contaminated equipment and insufficient hand hygiene practices among staff.
Table of Comparison
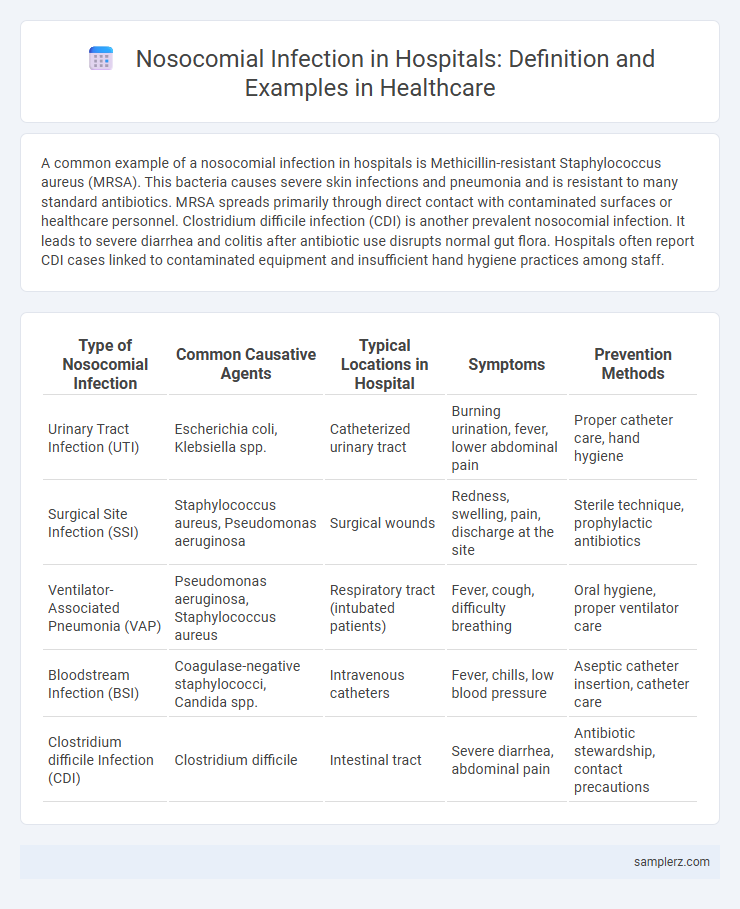
| Type of Nosocomial Infection | Common Causative Agents | Typical Locations in Hospital | Symptoms | Prevention Methods |
|---|---|---|---|---|
| Urinary Tract Infection (UTI) | Escherichia coli, Klebsiella spp. | Catheterized urinary tract | Burning urination, fever, lower abdominal pain | Proper catheter care, hand hygiene |
| Surgical Site Infection (SSI) | Staphylococcus aureus, Pseudomonas aeruginosa | Surgical wounds | Redness, swelling, pain, discharge at the site | Sterile technique, prophylactic antibiotics |
| Ventilator-Associated Pneumonia (VAP) | Pseudomonas aeruginosa, Staphylococcus aureus | Respiratory tract (intubated patients) | Fever, cough, difficulty breathing | Oral hygiene, proper ventilator care |
| Bloodstream Infection (BSI) | Coagulase-negative staphylococci, Candida spp. | Intravenous catheters | Fever, chills, low blood pressure | Aseptic catheter insertion, catheter care |
| Clostridium difficile Infection (CDI) | Clostridium difficile | Intestinal tract | Severe diarrhea, abdominal pain | Antibiotic stewardship, contact precautions |
Overview of Nosocomial Infections in Hospitals
Nosocomial infections, also known as hospital-acquired infections (HAIs), commonly include bloodstream infections, urinary tract infections, surgical site infections, and pneumonia, frequently caused by pathogens such as Staphylococcus aureus, Escherichia coli, and Pseudomonas aeruginosa. These infections occur in hospital settings due to factors like invasive procedures, contaminated medical equipment, and prolonged hospital stays, significantly impacting patient morbidity and healthcare costs. Effective infection control measures and surveillance systems are critical in minimizing the incidence of nosocomial infections and improving patient outcomes.
Common Types of Hospital-Acquired Infections
Common types of hospital-acquired infections include catheter-associated urinary tract infections (CAUTIs), surgical site infections (SSIs), bloodstream infections (BSIs), and ventilator-associated pneumonia (VAP). These infections are often caused by pathogens such as Staphylococcus aureus, Escherichia coli, Klebsiella pneumoniae, and Pseudomonas aeruginosa. Effective infection control measures and proper hygiene practices are essential to reduce the incidence of these nosocomial infections in healthcare settings.
Methicillin-Resistant Staphylococcus aureus (MRSA) Cases
Methicillin-Resistant Staphylococcus aureus (MRSA) is a prevalent example of a nosocomial infection in hospitals, often causing bloodstream infections, surgical site infections, and pneumonia. MRSA strains exhibit resistance to multiple antibiotics, complicating treatment and increasing hospital stay durations. Effective infection control measures and antibiotic stewardship programs are essential to reduce MRSA transmission and associated morbidity in healthcare settings.
Examples of Ventilator-Associated Pneumonia (VAP)
Ventilator-Associated Pneumonia (VAP) is a common nosocomial infection occurring in intubated patients within hospital intensive care units (ICUs). Pathogens such as Pseudomonas aeruginosa, Staphylococcus aureus (including MRSA), and Klebsiella pneumoniae are frequently identified as causative agents in VAP cases. Effective prevention strategies include strict adherence to ventilator care bundles, oral hygiene protocols, and minimizing the duration of mechanical ventilation.
Catheter-Associated Urinary Tract Infections (CAUTI)
Catheter-Associated Urinary Tract Infections (CAUTI) are among the most common nosocomial infections in hospitals, affecting patients with indwelling urinary catheters. These infections result from microbial colonization along the catheter, leading to symptoms such as dysuria, fever, and urinary urgency. Effective prevention strategies include aseptic catheter insertion, timely catheter removal, and adherence to strict infection control protocols.
Surgical Site Infection Examples in Clinical Settings
Surgical site infections (SSIs) commonly occur after procedures such as cesarean sections, orthopedic surgeries, and cardiac surgeries, often caused by bacteria like Staphylococcus aureus and Escherichia coli. These infections result from contamination during surgery or inadequate sterilization of instruments, leading to prolonged hospital stays and increased healthcare costs. Preventative measures including proper antiseptic techniques, antibiotic prophylaxis, and sterile operating environments significantly reduce the incidence of SSIs in clinical settings.
Clostridium difficile (C. diff) Infections in Hospitals
Clostridium difficile (C. diff) infections are a common nosocomial infection in hospitals, primarily affecting patients undergoing antibiotic treatment that disrupts normal gut flora. These infections cause severe diarrhea and colitis, often leading to prolonged hospital stays and increased healthcare costs. Rigorous infection control measures and antibiotic stewardship are essential to reduce the incidence of C. diff in healthcare settings.
Central Line-Associated Bloodstream Infection (CLABSI) Cases
Central Line-Associated Bloodstream Infection (CLABSI) represents a significant percentage of nosocomial infections, occurring when bacteria or viruses enter the bloodstream through a central line catheter. These infections increase hospital stay duration, healthcare costs, and patient mortality rates, with rates reported at 1.5 to 5 per 1,000 central line days in intensive care units. Effective prevention requires strict adherence to sterile techniques during line insertion and maintenance, as well as continuous staff education and infection control protocols.
Transmission Routes of Nosocomial Pathogens
Nosocomial infections commonly spread through direct contact with contaminated healthcare workers' hands, medical instruments, or surfaces within hospitals. Airborne transmission occurs via respiratory droplets, especially in cases involving pathogens like Mycobacterium tuberculosis or influenza virus. Other routes include the use of invasive devices such as catheters and ventilators, which can introduce pathogens like Staphylococcus aureus or Pseudomonas aeruginosa directly into sterile body sites.
Strategies to Prevent Nosocomial Infections in Healthcare
Hand hygiene protocols, such as regular handwashing with antimicrobial soap and the use of alcohol-based hand sanitizers, significantly reduce the transmission of nosocomial infections like Methicillin-resistant Staphylococcus aureus (MRSA) in hospitals. Sterilization of medical equipment combined with proper use of personal protective equipment (PPE) helps prevent the spread of pathogens including Clostridium difficile and bloodstream infections. Implementing isolation procedures for infected patients and continuous staff training on infection control practices are essential strategies to minimize healthcare-associated infections.
example of nosocomial infection in hospital Infographic
 samplerz.com
samplerz.com