Parenteral nutrition refers to the intravenous administration of nutrients directly into the bloodstream, bypassing the digestive system. An example of parenteral nutrition is Total Parenteral Nutrition (TPN), which provides essential nutrients such as glucose, amino acids, lipids, vitamins, and minerals to patients unable to consume or absorb food orally. TPN is commonly used in medical conditions like severe gastrointestinal disorders, postoperative recovery, or chronic bowel diseases. Healthcare providers monitor patients receiving parenteral nutrition closely to ensure proper nutrient balance and prevent complications such as infections or metabolic imbalances. Data shows that parenteral nutrition can be life-saving for individuals with compromised digestive function, supporting their nutritional needs while promoting healing. Advanced formulations of parenteral solutions are tailored to individual patient requirements based on factors like age, medical condition, and biochemical markers.
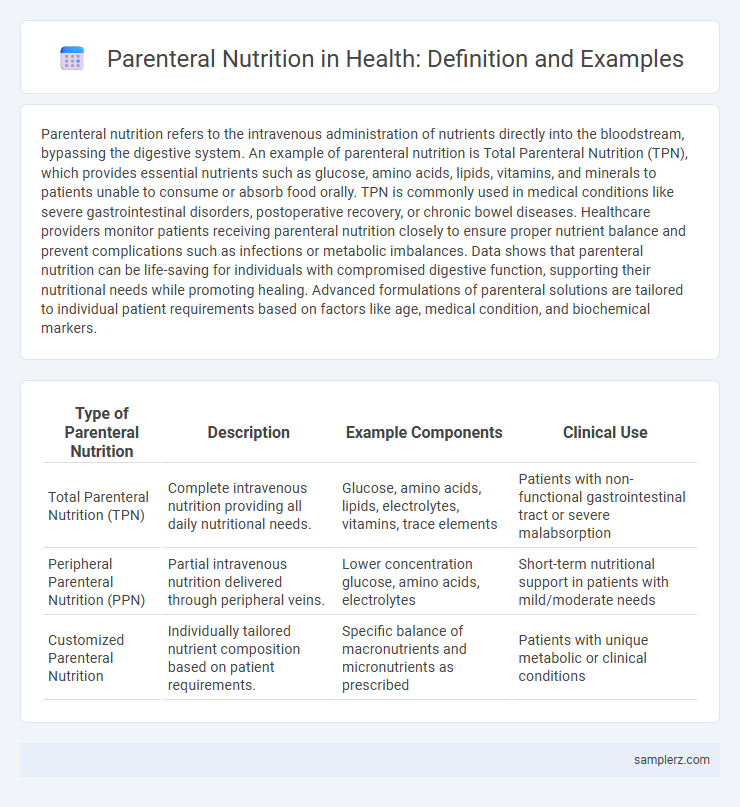
Table of Comparison
| Type of Parenteral Nutrition | Description | Example Components | Clinical Use |
|---|---|---|---|
| Total Parenteral Nutrition (TPN) | Complete intravenous nutrition providing all daily nutritional needs. | Glucose, amino acids, lipids, electrolytes, vitamins, trace elements | Patients with non-functional gastrointestinal tract or severe malabsorption |
| Peripheral Parenteral Nutrition (PPN) | Partial intravenous nutrition delivered through peripheral veins. | Lower concentration glucose, amino acids, electrolytes | Short-term nutritional support in patients with mild/moderate needs |
| Customized Parenteral Nutrition | Individually tailored nutrient composition based on patient requirements. | Specific balance of macronutrients and micronutrients as prescribed | Patients with unique metabolic or clinical conditions |
Understanding Parenteral Nutrition: An Overview
Parenteral nutrition delivers essential nutrients directly into the bloodstream through intravenous administration, bypassing the digestive system entirely. Common examples include Total Parenteral Nutrition (TPN), which provides a complete balance of amino acids, glucose, lipids, vitamins, and minerals to patients unable to consume or absorb food orally. This method supports individuals with gastrointestinal disorders, severe malabsorption, or post-surgical recovery requiring intensive nutritional support.
Key Components of Parenteral Nutrition Solutions
Parenteral nutrition solutions typically contain key components such as amino acids, dextrose, lipids, electrolytes, vitamins, and trace elements to meet the metabolic needs of patients unable to tolerate enteral feeding. Amino acids provide essential nitrogen for protein synthesis, while dextrose serves as the primary energy source. Lipid emulsions supply essential fatty acids and calories, and carefully balanced electrolytes and micronutrients ensure proper physiological function and prevent nutritional deficiencies.
Indications for Parenteral Nutrition Use
Parenteral nutrition is indicated for patients with non-functional or inaccessible gastrointestinal tracts, including cases such as bowel obstruction, severe pancreatitis, or short bowel syndrome. It is essential for individuals unable to meet nutrient requirements through oral or enteral feeding due to impaired digestion or absorption. Critical care settings also utilize parenteral nutrition to provide complete nutritional support during prolonged fasting or severe malnutrition.
Types of Parenteral Nutrition: TPN vs. PPN
Total Parenteral Nutrition (TPN) delivers all necessary nutrients intravenously, bypassing the gastrointestinal tract entirely, suitable for patients with severe digestive impairments. Peripheral Parenteral Nutrition (PPN) provides partial nutritional support through peripheral veins, ideal for short-term or less intensive needs. Both methods supply essential macronutrients and micronutrients tailored to patient-specific metabolic requirements in clinical settings.
Common Examples of Parenteral Nutrition Formulations
Common examples of parenteral nutrition formulations include total parenteral nutrition (TPN) solutions containing glucose, amino acids, lipids, vitamins, and trace elements. These formulations are tailored to meet individual patient needs, often combining dextrose as a primary energy source with intravenous lipid emulsions for essential fatty acids and protein synthesis. Electrolyte balance and micronutrient supplementation are critical components to support metabolic functions during parenteral feeding.
Administration Methods for Parenteral Nutrition
Parenteral nutrition is primarily administered through central venous catheters, including peripherally inserted central catheters (PICC lines) and tunneled central veins, which deliver nutrient-rich solutions directly into the bloodstream for patients unable to use the gastrointestinal tract. Peripheral parenteral nutrition involves short-term administration via peripheral veins, typically suitable for less concentrated solutions to avoid vein irritation. Techniques such as continuous infusion using infusion pumps optimize nutrient delivery and reduce complications like infection or thrombosis.
Monitoring and Managing Parenteral Nutrition Therapy
Parenteral nutrition therapy requires continuous monitoring of electrolyte levels, fluid balance, and blood glucose to prevent complications such as infections, metabolic imbalances, and liver dysfunction. Regular assessment of catheter site integrity and aseptic technique is essential to reduce the risk of bloodstream infections. Advanced monitoring tools, including biochemical markers and volumetric devices, support precise adjustment of nutrient composition tailored to individual patient needs.
Risks and Complications of Parenteral Nutrition
Parenteral nutrition carries significant risks including bloodstream infections, metabolic imbalances such as hyperglycemia or electrolyte disturbances, and liver dysfunction. Catheter-related complications like thrombosis and mechanical issues pose additional threats to patient safety. Careful monitoring and strict aseptic techniques are essential to minimize these potentially serious complications during parenteral feeding.
Benefits of Parenteral Nutrition for Patient Recovery
Parenteral nutrition delivers essential nutrients directly into the bloodstream, bypassing the digestive tract, which is critical for patients with impaired gastrointestinal function. This method provides customized nutrient formulations tailored to individual metabolic needs, enhancing recovery speed and reducing the risk of malnutrition-related complications. By ensuring precise hydration and electrolyte balance, parenteral nutrition supports optimal organ function and accelerates overall patient healing.
Innovations in Parenteral Nutrition Practices
Innovations in parenteral nutrition practices include the development of multi-chamber bags combining amino acids, lipids, and glucose to reduce contamination risk and improve nutrient stability. Advanced infusion pumps with real-time monitoring and adjustable flow rates enhance precision in nutrient delivery for critically ill patients. Novel lipid emulsions enriched with omega-3 fatty acids demonstrate improved anti-inflammatory effects and better clinical outcomes in total parenteral nutrition therapy.
example of parenteral in nutrition Infographic
 samplerz.com
samplerz.com