Diathesis in mental illness refers to an individual's predisposition or vulnerability to develop a psychiatric disorder due to genetic, biological, or environmental factors. For example, a person with a family history of schizophrenia may have a genetic diathesis, increasing their risk of developing the condition under stressful circumstances. This predisposition interacts with external stressors, contributing to the onset and severity of mental health disorders. Research in mental health highlights the role of diathesis-stress models in understanding illnesses like depression and bipolar disorder. People with a genetic diathesis may experience biochemical imbalances or neurodevelopmental differences that make them susceptible to these conditions. Identifying diathesis allows clinicians to tailor preventive interventions and personalized treatment strategies based on individual risk profiles.
Table of Comparison
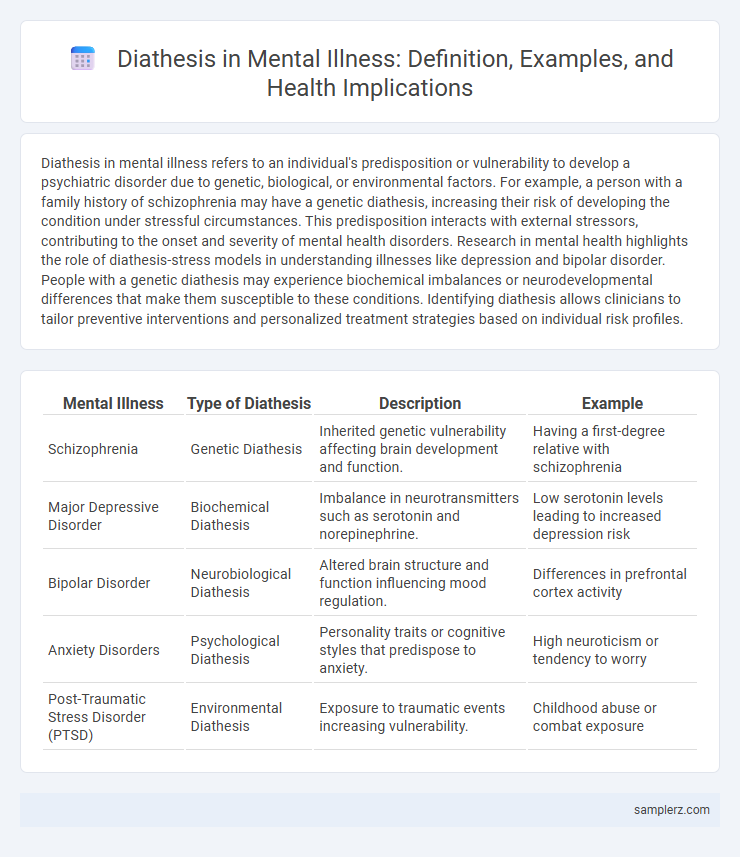
| Mental Illness | Type of Diathesis | Description | Example |
|---|---|---|---|
| Schizophrenia | Genetic Diathesis | Inherited genetic vulnerability affecting brain development and function. | Having a first-degree relative with schizophrenia |
| Major Depressive Disorder | Biochemical Diathesis | Imbalance in neurotransmitters such as serotonin and norepinephrine. | Low serotonin levels leading to increased depression risk |
| Bipolar Disorder | Neurobiological Diathesis | Altered brain structure and function influencing mood regulation. | Differences in prefrontal cortex activity |
| Anxiety Disorders | Psychological Diathesis | Personality traits or cognitive styles that predispose to anxiety. | High neuroticism or tendency to worry |
| Post-Traumatic Stress Disorder (PTSD) | Environmental Diathesis | Exposure to traumatic events increasing vulnerability. | Childhood abuse or combat exposure |
Defining Diathesis in the Context of Mental Illness
Diathesis in mental illness refers to an underlying vulnerability or predisposition that increases an individual's risk of developing a psychiatric disorder, often triggered by environmental stressors. This genetic or biological susceptibility interacts with external factors, such as trauma or chronic stress, to contribute to conditions like depression, schizophrenia, or anxiety disorders. Understanding diathesis helps in identifying at-risk individuals and tailoring preventative or therapeutic interventions.
The Diathesis-Stress Model Explained
The diathesis-stress model explains how genetic or biological predispositions, known as diatheses, interact with environmental stressors to trigger mental illnesses such as depression, anxiety, and schizophrenia. For example, individuals with a family history of bipolar disorder may remain symptom-free until significant life stressors activate the underlying vulnerability. This model emphasizes the dynamic interplay between inherited risks and external pressures in the development and progression of psychiatric conditions.
Genetic Predispositions as Diatheses
Genetic predispositions serve as critical diatheses in mental illness, influencing susceptibility to disorders such as schizophrenia, bipolar disorder, and major depressive disorder. Specific gene variants like DISC1 and COMT have been linked to increased risk, highlighting the biological basis of psychiatric conditions. Studies of twin concordance rates underscore the heritable nature of these illnesses, supporting the diathesis-stress model in psychiatric genetics.
Childhood Trauma and Early Life Experiences
Childhood trauma, including physical, emotional, or sexual abuse, is a significant diathesis influencing the development of mental illnesses such as depression and post-traumatic stress disorder (PTSD). Early life experiences characterized by neglect or inconsistent caregiving disrupt neurodevelopment, increasing vulnerability to anxiety disorders and borderline personality disorder. These adverse events interact with genetic predispositions, amplifying the risk of long-term psychiatric conditions.
Biological Vulnerabilities in Mental Disorders
Biological vulnerabilities in mental disorders include genetic predispositions, neurochemical imbalances, and structural brain abnormalities that increase the risk of conditions like schizophrenia and bipolar disorder. For example, a diathesis in schizophrenia often involves dopamine dysregulation combined with genetic mutations in genes such as COMT and DISC1. These inherent biological factors interact with environmental stressors, triggering the onset and progression of mental illness.
Cognitive Styles and Thought Patterns
Diathesis in mental illness often manifests through maladaptive cognitive styles such as negative attributional bias and rumination, which predispose individuals to disorders like depression and anxiety. Thought patterns characterized by cognitive distortions, including catastrophizing and black-and-white thinking, increase vulnerability to psychopathology by reinforcing emotional dysregulation. Understanding these cognitive diatheses enables targeted interventions such as cognitive-behavioral therapy to modify dysfunctional thinking and reduce relapse risk.
Family History as a Risk Factor
Family history significantly increases the risk of developing mental illnesses such as schizophrenia, bipolar disorder, and major depressive disorder due to inherited genetic vulnerabilities known as diathesis. Research shows that individuals with first-degree relatives affected by these conditions have a two to four times higher likelihood of exhibiting similar psychiatric symptoms. This genetic predisposition, combined with environmental stressors, contributes to the manifestation of mental health disorders.
Environmental Influences on Diathesis
Exposure to chronic stress, traumatic events, and adverse childhood experiences exemplify environmental influences on diathesis in mental illness, increasing vulnerability to disorders such as depression and anxiety. These environmental stressors interact with genetic predispositions to trigger or exacerbate mental health conditions. Socioeconomic factors, including poverty and social isolation, further compound the diathesis, highlighting the critical role of external environments in the pathogenesis of mental disorders.
Neurochemical Imbalances and Mental Illness
Neurochemical imbalances, such as dysregulated serotonin and dopamine levels, exemplify a diathesis contributing to mental illnesses like depression and schizophrenia. These imbalances disrupt neural communication and mood regulation, increasing vulnerability to psychiatric disorders. Understanding this biological predisposition aids in targeted pharmacological treatments for symptom management.
Case Studies: Diathesis in Real-World Mental Health Scenarios
Case studies in psychiatry often highlight the diathesis-stress model to explain disorders such as schizophrenia and major depressive disorder; for instance, individuals with a genetic predisposition to schizophrenia may develop symptoms after significant environmental stressors like trauma or substance abuse. Analysis of bipolar disorder reveals that a family history of mood disorders combined with stressful life events increases the likelihood of onset and relapse. These case studies emphasize the interaction between inherent vulnerability and external stressors in triggering mental health conditions, guiding personalized treatment approaches.
example of diathesis in mental illness Infographic
 samplerz.com
samplerz.com