Orthostatic hypotension is a common cardiovascular condition characterized by a significant drop in blood pressure upon standing. In cardiology, it is often observed in patients with autonomic dysfunction, including those with heart failure or postural tachycardia syndrome (POTS). This condition can result in dizziness, fainting, and increased risk of falls due to impaired cerebral perfusion. Data from clinical studies indicate that orthostatic hypotension affects approximately 6-30% of elderly patients with cardiovascular disease. Diagnostic criteria typically include a systolic blood pressure decrease of at least 20 mm Hg or a diastolic decrease of 10 mm Hg within three minutes of standing. Management strategies focus on medication adjustments, hydration, and physical counter-maneuvers to improve blood pressure regulation.
Table of Comparison
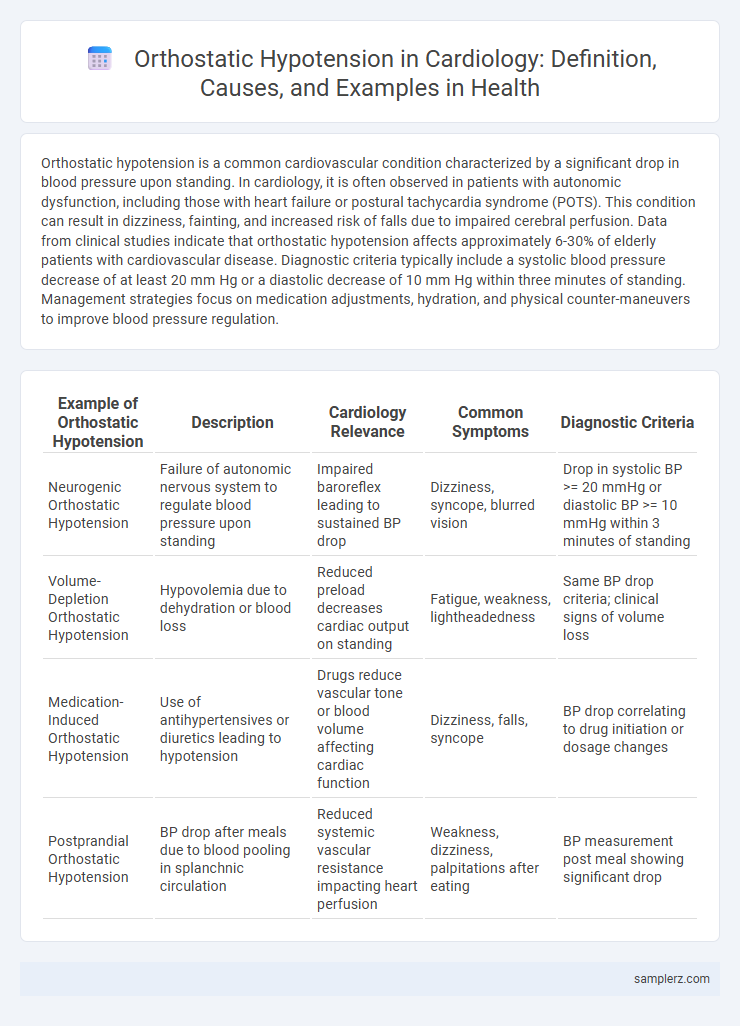
| Example of Orthostatic Hypotension | Description | Cardiology Relevance | Common Symptoms | Diagnostic Criteria |
|---|---|---|---|---|
| Neurogenic Orthostatic Hypotension | Failure of autonomic nervous system to regulate blood pressure upon standing | Impaired baroreflex leading to sustained BP drop | Dizziness, syncope, blurred vision | Drop in systolic BP >= 20 mmHg or diastolic BP >= 10 mmHg within 3 minutes of standing |
| Volume- Depletion Orthostatic Hypotension | Hypovolemia due to dehydration or blood loss | Reduced preload decreases cardiac output on standing | Fatigue, weakness, lightheadedness | Same BP drop criteria; clinical signs of volume loss |
| Medication-Induced Orthostatic Hypotension | Use of antihypertensives or diuretics leading to hypotension | Drugs reduce vascular tone or blood volume affecting cardiac function | Dizziness, falls, syncope | BP drop correlating to drug initiation or dosage changes |
| Postprandial Orthostatic Hypotension | BP drop after meals due to blood pooling in splanchnic circulation | Reduced systemic vascular resistance impacting heart perfusion | Weakness, dizziness, palpitations after eating | BP measurement post meal showing significant drop |
Understanding Orthostatic Hypotension in Cardiology
Orthostatic hypotension in cardiology manifests as a significant drop in blood pressure upon standing, typically exceeding a 20 mmHg decrease in systolic pressure or 10 mmHg in diastolic pressure within three minutes. This condition often results from impaired autonomic regulation of cardiovascular function, leading to symptoms such as dizziness, syncope, and increased risk of falls. Recognizing orthostatic hypotension is critical in managing patients with heart failure, arrhythmias, or those on antihypertensive medications to prevent adverse cardiovascular events.
Common Symptoms of Orthostatic Hypotension
Orthostatic hypotension commonly presents with symptoms such as dizziness, lightheadedness, and blurred vision upon standing. Patients may also experience fatigue, weakness, and palpitations due to decreased cerebral perfusion. These signs are crucial indicators for cardiologists to evaluate blood pressure regulation and autonomic nervous system function.
Clinical Presentation in Cardiac Patients
Orthostatic hypotension in cardiac patients commonly presents with dizziness, lightheadedness, and syncope upon standing, often linked to impaired autonomic regulation or reduced cardiac output. Symptoms can exacerbate pre-existing heart conditions such as heart failure or arrhythmias, compromising cerebral perfusion. Clinical evaluation includes blood pressure measurements in supine and standing positions, with a drop of at least 20 mmHg systolic or 10 mmHg diastolic within three minutes confirming diagnosis.
Key Causes of Orthostatic Hypotension in Heart Disease
Orthostatic hypotension in cardiology often results from impaired autonomic regulation due to heart failure, which reduces cardiac output and compromises blood pressure stability upon standing. Medications commonly used in heart disease, such as beta-blockers and diuretics, contribute to this condition by decreasing vascular tone and blood volume. Autonomic neuropathy in patients with ischemic heart disease further impairs baroreflex sensitivity, exacerbating orthostatic blood pressure drops.
Diagnostic Criteria for Orthostatic Hypotension
Orthostatic hypotension in cardiology is diagnosed by a sustained drop in systolic blood pressure of at least 20 mmHg or diastolic blood pressure of 10 mmHg within three minutes of standing from a supine position. Heart rate changes are also assessed to differentiate neurogenic causes from hypovolemic or medication-induced hypotension. Continuous blood pressure monitoring and tilt-table tests enhance diagnostic accuracy in clinical evaluation.
Case Study: Orthostatic Hypotension in Cardiomyopathy
Orthostatic hypotension in cardiomyopathy often presents with significant drops in blood pressure upon standing, leading to dizziness and syncope due to impaired cardiac output. A case study involving a patient with dilated cardiomyopathy revealed recurrent episodes of hypotension linked to autonomic dysfunction exacerbated by reduced left ventricular ejection fraction. Management strategies included volume expansion and pharmacologic agents such as midodrine to stabilize blood pressure and improve orthostatic tolerance in cardiomyopathic patients.
Impact of Orthostatic Hypotension on Cardiac Function
Orthostatic hypotension significantly impacts cardiac function by reducing cerebral perfusion and triggering compensatory tachycardia to maintain blood pressure, which can exacerbate underlying heart conditions. Patients with impaired autonomic regulation, such as those with heart failure or arrhythmias, experience increased morbidity due to the stress imposed on the myocardium during postural changes. Monitoring orthostatic blood pressure variations is essential for optimizing therapeutic strategies and preventing adverse cardiovascular events in these populations.
Pharmacological Triggers in Cardiac Patients
Orthostatic hypotension in cardiology often occurs in cardiac patients due to pharmacological triggers such as beta-blockers, diuretics, and vasodilators, which can impair blood pressure regulation. These medications reduce cardiac output or induce vascular dilation, exacerbating blood pooling in the lower extremities upon standing. Careful management of drug regimens and monitoring for hypotensive symptoms are essential to prevent syncope and falls in cardiac patients.
Management Strategies in Cardiology Practice
Management strategies for orthostatic hypotension in cardiology practice include the use of volume expansion through increased salt and fluid intake, along with pharmacologic treatments such as midodrine and fludrocortisone to improve vascular tone. Physical counterpressure maneuvers, including leg crossing and squatting, are recommended to reduce symptom severity by enhancing venous return. Continuous monitoring of blood pressure changes during positional shifts and patient education on lifestyle modifications play critical roles in optimizing therapeutic outcomes.
Preventive Measures for Cardiac Patients at Risk
Orthostatic hypotension in cardiology often affects cardiac patients who experience a sudden drop in blood pressure upon standing, increasing the risk of dizziness and falls. Preventive measures include gradual position changes, adequate hydration, and medication adjustments tailored to minimize blood pressure fluctuations. Regular monitoring and physical therapy can also enhance vascular tone and autonomic function, reducing orthostatic hypotension episodes in high-risk cardiac patients.
example of orthostatic hypotension in cardiology Infographic
 samplerz.com
samplerz.com