Apraxia is a neurological disorder often observed in stroke patients, characterized by the inability to perform purposeful movements despite having the physical ability and desire to do so. For example, a stroke survivor with limb apraxia may struggle to brush their hair or button a shirt, even though their muscles function normally. This condition results from damage to specific brain regions, such as the parietal lobe or premotor cortex, which disrupts motor planning and coordination. Data shows that apraxia affects approximately 30-50% of individuals recovering from a stroke, impacting their daily living activities and independence. Diagnosis involves clinical assessments like the Apraxia Screen of TULIA or the Florida Apraxia Screening Test, focusing on gesture imitation and tool use. Rehabilitation includes occupational therapy targeting motor planning skills to help patients regain functional movement and improve quality of life.
Table of Comparison
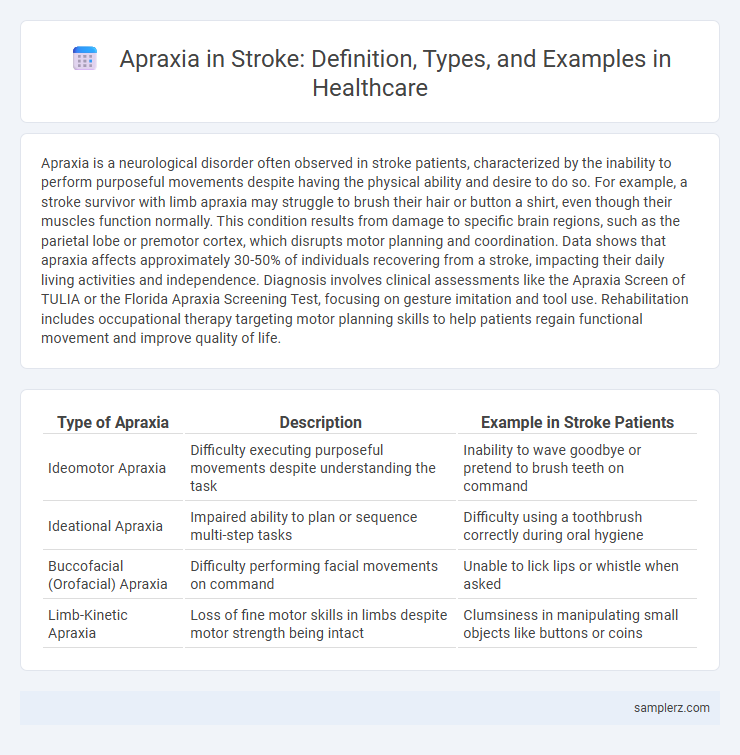
| Type of Apraxia | Description | Example in Stroke Patients |
|---|---|---|
| Ideomotor Apraxia | Difficulty executing purposeful movements despite understanding the task | Inability to wave goodbye or pretend to brush teeth on command |
| Ideational Apraxia | Impaired ability to plan or sequence multi-step tasks | Difficulty using a toothbrush correctly during oral hygiene |
| Buccofacial (Orofacial) Apraxia | Difficulty performing facial movements on command | Unable to lick lips or whistle when asked |
| Limb-Kinetic Apraxia | Loss of fine motor skills in limbs despite motor strength being intact | Clumsiness in manipulating small objects like buttons or coins |
Understanding Apraxia: Definition and Types
Apraxia is a neurological disorder characterized by the inability to perform purposeful movements despite having the physical ability and desire to do so, commonly observed after a stroke affecting the left hemisphere of the brain. Types of apraxia include ideomotor apraxia, where patients struggle with executing simple gestures on command, and ideational apraxia, involving difficulty planning a sequence of actions required to complete complex tasks. Stroke-induced apraxia often results from damage to the parietal or frontal lobes, impairing motor planning and coordination essential for daily activities.
How Stroke Leads to Apraxia
Stroke causes apraxia by damaging the brain regions responsible for motor planning, particularly in the left hemisphere's parietal or frontal lobes. Lesions in these areas disrupt the neural pathways needed to coordinate purposeful movements, leading to difficulties in performing tasks despite intact muscle function. This impairment results in the inability to execute learned motor skills, which is characteristic of apraxia after a stroke.
Common Signs of Apraxia in Stroke Survivors
Common signs of apraxia in stroke survivors include difficulty performing purposeful movements despite intact motor function, such as struggling to wave goodbye or use utensils correctly. Patients often exhibit impaired ability to sequence or imitate gestures, leading to challenges in daily activities like dressing or brushing teeth. These symptoms arise from brain damage affecting motor planning areas, notably the left parietal lobe.
Limb Apraxia: Difficulty with Movement After Stroke
Limb apraxia, a common post-stroke condition, impairs a person's ability to perform purposeful movements despite having the physical strength and coordination to do so. This difficulty occurs because stroke can damage the brain regions responsible for planning and executing motor tasks, particularly in the left parietal lobe. Patients with limb apraxia may struggle to carry out everyday activities such as waving goodbye, using utensils, or buttoning a shirt, which significantly impacts their independence.
Speech Apraxia: Challenges in Verbal Communication
Speech apraxia, a common manifestation following a stroke, impairs the brain's ability to plan and coordinate the muscle movements necessary for clear speech. Patients often struggle to pronounce words correctly, leading to fragmented and inconsistent verbal communication despite understanding language and having intact muscle strength. This disruption significantly affects social interactions and rehabilitation progress, necessitating targeted speech therapy for recovery.
Daily Activities Affected by Apraxia Post-Stroke
Apraxia post-stroke significantly impairs daily activities such as dressing, eating, and grooming, where patients struggle to sequence and execute motor tasks despite having intact muscle strength. Tasks like buttoning a shirt or using utensils become challenging due to disrupted motor planning pathways in the parietal and frontal lobes. Rehabilitation targeting praxis skills is crucial to regain independence and improve quality of life for stroke survivors experiencing apraxia.
Apraxia vs. Other Neurological Disorders
Apraxia in stroke patients is characterized by an impaired ability to perform purposeful movements despite intact motor and sensory function, often differentiating it from other neurological disorders such as aphasia or ataxia. Unlike aphasia, which affects language processing, apraxia primarily disrupts motor planning and execution without compromising comprehension or muscle strength. Distinguishing apraxia from movement disorders like Parkinson's disease or hemiparesis post-stroke aids in accurate diagnosis and targeted rehabilitation strategies.
Assessment Tools for Diagnosing Apraxia in Stroke Patients
Assessment tools for diagnosing apraxia in stroke patients include the Apraxia Screen of Stroke (ASS), which efficiently evaluates limb and oral praxis using standardized tasks. The Florida Apraxia Battery provides a comprehensive examination by assessing gesture production and imitation critical for identifying specific apraxic deficits. Neuropsychological tests combined with functional imaging techniques such as fMRI enhance diagnostic accuracy by correlating clinical symptoms with affected brain regions.
Rehabilitation Strategies for Apraxia Following Stroke
Rehabilitation strategies for apraxia following stroke involve task-specific training that targets improving motor planning and execution through repetitive, guided practice of everyday actions such as dressing and using utensils. Incorporating motor imagery and gesture training enhances neural reorganization, while occupational therapy focuses on adapting activities to the patient's current capabilities to promote independence. Evidence supports the use of virtual reality and augmented reality tools to provide immersive, interactive environments that facilitate motor relearning and increase patient motivation during therapy sessions.
Support Resources for Stroke Survivors with Apraxia
Support resources for stroke survivors with apraxia include specialized speech-language therapy that targets motor planning and coordination of movements. Technological aids such as gesture recognition apps and communication devices enhance daily interaction and improve functional independence. Support groups and rehabilitation programs offer emotional assistance and practical strategies, fostering better coping mechanisms for managing apraxic challenges post-stroke.
example of apraxia in stroke Infographic
 samplerz.com
samplerz.com