Iatrogenesis in surgical procedures refers to adverse conditions or complications caused unintentionally by medical treatment or surgical interventions. An example is surgical site infections (SSI), which occur when bacteria enter the wound during or after surgery, leading to inflammation, pain, and prolonged recovery. These infections are significant contributors to postoperative morbidity and can increase healthcare costs and hospital stays. Another example includes nerve damage during orthopedic surgeries, such as hip or shoulder replacements, where accidental injury to surrounding nerves results in numbness, weakness, or chronic pain. Iatrogenic bleeding can also arise from improper handling of blood vessels during operations, causing excessive blood loss and necessitating transfusions or additional surgical intervention. Monitoring surgical techniques and using sterile environments helps minimize the risks associated with iatrogenesis in surgical procedures.
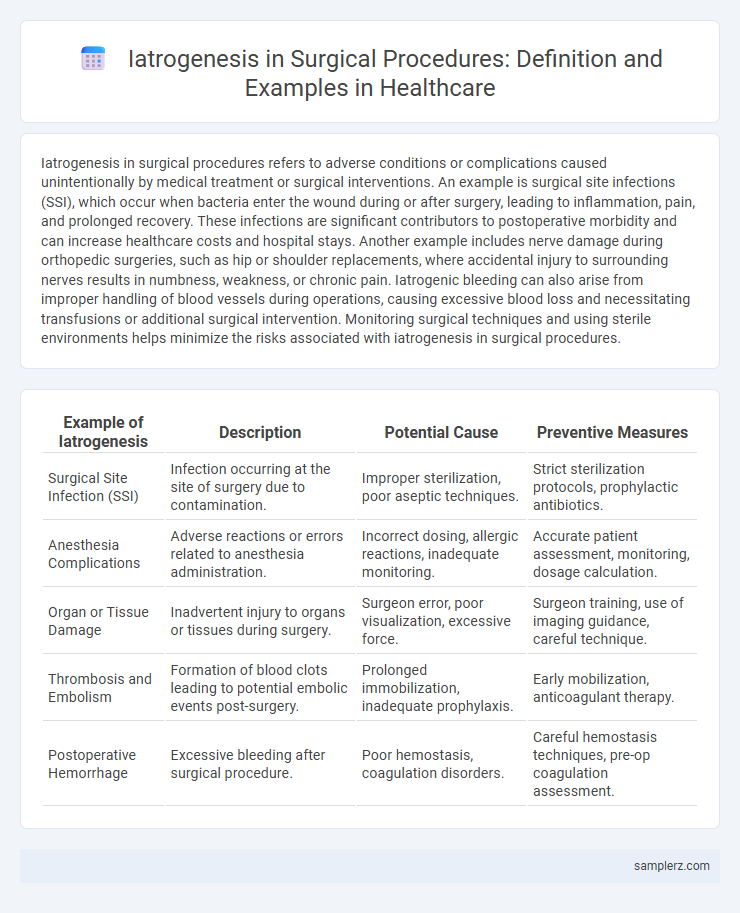
Table of Comparison
| Example of Iatrogenesis | Description | Potential Cause | Preventive Measures |
|---|---|---|---|
| Surgical Site Infection (SSI) | Infection occurring at the site of surgery due to contamination. | Improper sterilization, poor aseptic techniques. | Strict sterilization protocols, prophylactic antibiotics. |
| Anesthesia Complications | Adverse reactions or errors related to anesthesia administration. | Incorrect dosing, allergic reactions, inadequate monitoring. | Accurate patient assessment, monitoring, dosage calculation. |
| Organ or Tissue Damage | Inadvertent injury to organs or tissues during surgery. | Surgeon error, poor visualization, excessive force. | Surgeon training, use of imaging guidance, careful technique. |
| Thrombosis and Embolism | Formation of blood clots leading to potential embolic events post-surgery. | Prolonged immobilization, inadequate prophylaxis. | Early mobilization, anticoagulant therapy. |
| Postoperative Hemorrhage | Excessive bleeding after surgical procedure. | Poor hemostasis, coagulation disorders. | Careful hemostasis techniques, pre-op coagulation assessment. |
Common Types of Iatrogenic Injuries in Surgery
Common types of iatrogenic injuries in surgery include nerve damage, surgical site infections, and unintended organ perforations. These complications often arise from technical errors, such as improper incision or instrument use, and can lead to prolonged recovery, additional surgeries, or chronic pain. Effective prevention relies on strict adherence to surgical protocols, thorough preoperative planning, and continuous intraoperative monitoring.
Surgical Site Infections as Iatrogenic Complications
Surgical site infections (SSIs) represent a common example of iatrogenic complications that occur due to microbial contamination during or after surgical procedures. These infections contribute significantly to postoperative morbidity, prolonged hospital stays, and increased healthcare costs. Effective prevention strategies include strict adherence to aseptic techniques, appropriate prophylactic antibiotic administration, and meticulous wound care.
Iatrogenic Nerve Damage During Operations
Iatrogenic nerve damage during surgical procedures frequently occurs in operations involving the spine, shoulder, or pelvic region, leading to partial or complete loss of motor or sensory function. Commonly affected nerves include the radial nerve in humeral fractures, the peroneal nerve in knee surgeries, and the brachial plexus during clavicle repair. Recognizing high-risk surgeries and implementing nerve monitoring techniques reduces the incidence of such complications, improving patient outcomes.
Medication Errors in the Operating Room
Medication errors in the operating room represent a significant example of iatrogenesis, often involving incorrect drug dosages, wrong medications, or administration errors during surgery. These mistakes can lead to severe complications such as adverse drug reactions, prolonged hospital stays, or increased morbidity rates. Implementing standardized medication protocols and real-time verification systems are critical to minimizing the risk of iatrogenic harm in surgical settings.
Iatrogenic Bleeding and Hemorrhage During Surgery
Iatrogenic bleeding and hemorrhage during surgery represent critical complications where inadvertent damage to blood vessels occurs, leading to significant blood loss. Common causes include accidental vessel laceration, inadequate hemostasis, and surgical instrument trauma, often requiring immediate intervention such as vessel ligation or transfusion. Effective surgical techniques and intraoperative monitoring are essential to minimize the risk and manage these iatrogenic events promptly to prevent morbidity and mortality.
Surgical Instrument Retention: A Preventable Iatrogenic Error
Surgical instrument retention is a critical example of iatrogenesis, where tools or materials used during surgery are accidentally left inside a patient's body, leading to severe complications such as infections, pain, and the need for additional surgeries. This preventable error is primarily caused by lapses in counting protocols and inadequate surgical team communication. Implementing strict surgical safety checklists and advanced tracking technologies significantly reduces the incidence of retained surgical items, enhancing patient safety and outcomes.
Iatrogenic Organ Damage During Surgical Procedures
Iatrogenic organ damage during surgical procedures occurs when unintended injury to organs such as the bowel, bladder, or blood vessels results from surgical intervention. Common examples include bowel perforation during laparoscopic surgery and ureteral injury during hysterectomy. These complications often lead to increased morbidity, prolonged hospital stays, and additional corrective surgeries, highlighting the importance of precision and vigilance in operative techniques.
Postoperative Respiratory Complications Induced by Surgery
Postoperative respiratory complications such as pneumonia, atelectasis, and respiratory failure frequently arise as iatrogenic effects following surgical procedures, especially in patients undergoing thoracic or upper abdominal surgery. These complications result from factors including anesthesia-induced respiratory depression, impaired cough reflex, and prolonged immobilization. Early interventions like incentive spirometry, adequate pain control, and respiratory physiotherapy are essential to mitigate the morbidity and mortality associated with these iatrogenic respiratory events.
Iatrogenic Anesthesia-related Adverse Events
Iatrogenic anesthesia-related adverse events include complications such as airway injury, anesthesia awareness, and adverse drug reactions during surgical procedures. These events can lead to respiratory distress, allergic responses, or hemodynamic instability, significantly impacting patient outcomes. Proper anesthesia management and monitoring protocols are essential to minimize risks associated with anesthesia-induced iatrogenesis.
Preventive Strategies to Reduce Iatrogenesis in Surgery
Surgical site infections and unintended tissue damage are common examples of iatrogenesis in surgical procedures, often resulting from inadequate sterilization or procedural errors. Preventive strategies include strict adherence to aseptic techniques, comprehensive surgical checklists, and ongoing staff training to minimize human error. Implementation of advanced monitoring systems during surgery also helps detect complications early, reducing the risk of adverse outcomes.
example of iatrogenesis in surgical procedure Infographic
 samplerz.com
samplerz.com