Dysphagia is a common complication in stroke patients, characterized by difficulty in swallowing due to impaired neural control. This condition often results from damage to the brain areas responsible for coordinating the muscles involved in swallowing. Clinical manifestations include coughing, choking, and aspiration pneumonia, which pose significant risks to patient health and recovery. Stroke-induced dysphagia primarily affects the oropharyngeal phase of swallowing, leading to reduced efficiency and safety during food intake. Assessment methods such as video fluoroscopic swallow study (VFSS) and fiberoptic endoscopic evaluation of swallowing (FEES) provide valuable data for diagnosis. Early identification and management of dysphagia are critical to prevent malnutrition and respiratory complications, improving overall patient outcomes.
Table of Comparison
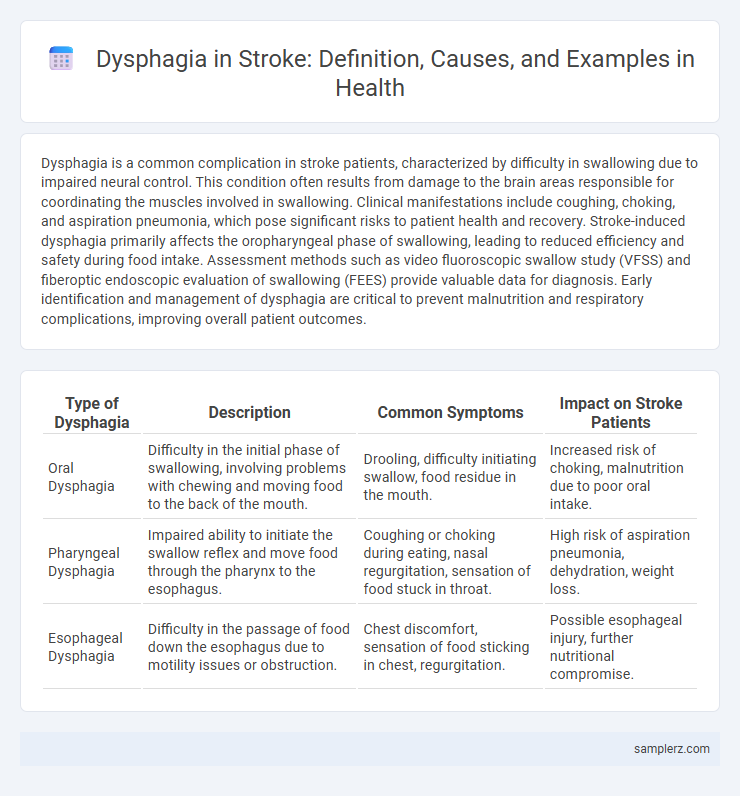
| Type of Dysphagia | Description | Common Symptoms | Impact on Stroke Patients |
|---|---|---|---|
| Oral Dysphagia | Difficulty in the initial phase of swallowing, involving problems with chewing and moving food to the back of the mouth. | Drooling, difficulty initiating swallow, food residue in the mouth. | Increased risk of choking, malnutrition due to poor oral intake. |
| Pharyngeal Dysphagia | Impaired ability to initiate the swallow reflex and move food through the pharynx to the esophagus. | Coughing or choking during eating, nasal regurgitation, sensation of food stuck in throat. | High risk of aspiration pneumonia, dehydration, weight loss. |
| Esophageal Dysphagia | Difficulty in the passage of food down the esophagus due to motility issues or obstruction. | Chest discomfort, sensation of food sticking in chest, regurgitation. | Possible esophageal injury, further nutritional compromise. |
Understanding Dysphagia After Stroke
Dysphagia after stroke commonly presents as difficulty swallowing due to impaired coordination of the muscles in the mouth, throat, and esophagus. This condition increases the risk of aspiration pneumonia and malnutrition, highlighting the need for early assessment using tools like the Gugging Swallowing Screen or videofluoroscopic swallow study. Effective management includes targeted swallowing therapy and dietary modifications to improve patient outcomes and reduce complications.
Common Types of Swallowing Difficulties in Stroke Survivors
Stroke survivors often experience oropharyngeal dysphagia, characterized by difficulty initiating a swallow due to impaired tongue and throat muscle coordination. Esophageal dysphagia, involving the disruption of food passage through the esophagus, also commonly occurs after stroke. These swallowing difficulties increase the risk of aspiration pneumonia, malnutrition, and dehydration in affected individuals.
Signs and Symptoms of Post-Stroke Dysphagia
Post-stroke dysphagia commonly presents with signs such as coughing or choking during meals, drooling, and changes in voice quality due to aspiration. Patients may experience difficulty initiating swallowing, sensation of food sticking in the throat, and prolonged mealtime duration. Early identification of these symptoms is crucial to prevent complications like malnutrition, dehydration, and pneumonia.
Neurological Causes of Dysphagia Following Stroke
Dysphagia following a stroke commonly results from neurological damage affecting the brainstem, corticobulbar pathways, or cranial nerves IX and X, which are critical for swallowing coordination. Lesions in the medulla oblongata disrupt the swallowing reflex, while cortical strokes impair voluntary initiation and control of swallowing muscles. Post-stroke dysphagia increases the risk of aspiration pneumonia, malnutrition, and dehydration, necessitating prompt assessment and intervention by speech-language pathologists.
Real-Life Case Studies: Dysphagia in Stroke Patients
A 68-year-old male stroke patient exhibited severe dysphagia, struggling with both oral and pharyngeal phases of swallowing, leading to frequent aspiration pneumonia. Video fluoroscopic swallowing study (VFSS) confirmed delayed swallow reflex and reduced laryngeal elevation, critical indicators for dysphagia severity in post-stroke individuals. Targeted swallowing therapy and dietary modifications significantly improved nutritional status and reduced respiratory complications in this case.
Impact of Dysphagia on Nutrition and Hydration
Dysphagia in stroke patients commonly leads to impaired swallowing function, significantly increasing the risk of malnutrition and dehydration. Inability to swallow effectively causes reduced oral intake of essential nutrients and fluids, which exacerbates muscle weakness and delays recovery. Nutritional interventions, such as modified texture diets and enteral feeding, are critical to maintaining adequate hydration and supporting rehabilitation outcomes.
Diagnostic Methods for Dysphagia in Stroke Patients
Diagnostic methods for dysphagia in stroke patients include the Bedside Swallowing Assessment, which evaluates swallowing function through clinical observation and patient history. Instrumental techniques such as Videofluoroscopic Swallowing Study (VFSS) and Fiberoptic Endoscopic Evaluation of Swallowing (FEES) provide detailed visualization of swallowing mechanics and identify aspiration risks. These tools are critical for tailored rehabilitation strategies and preventing complications like aspiration pneumonia.
Effective Treatment Strategies for Post-Stroke Dysphagia
Post-stroke dysphagia often results from impaired swallowing reflex due to brain damage affecting the corticobulbar tract, leading to risks such as aspiration pneumonia and malnutrition. Effective treatment strategies include targeted swallowing therapy incorporating exercises like the Mendelsohn maneuver and neuromuscular electrical stimulation to enhance muscle coordination and strength. Nutritional management with texture-modified diets and careful monitoring by speech-language pathologists significantly reduce complications and improve patient outcomes.
Rehabilitation Techniques to Improve Swallowing
Dysphagia following a stroke often results from impaired neural control of swallowing muscles, causing difficulties in safely managing oral intake. Rehabilitation techniques such as oropharyngeal exercises, neuromuscular electrical stimulation (NMES), and swallowing maneuvers like the Mendelsohn maneuver enhance muscle strength and coordination. Tailored therapy plans and use of biofeedback mechanisms contribute significantly to restoring effective swallowing function and reducing aspiration risks.
Preventing Complications: Aspiration Pneumonia and Beyond
Dysphagia after a stroke significantly increases the risk of aspiration pneumonia, a leading cause of morbidity and mortality in stroke survivors. Implementing early swallowing assessments and tailored rehabilitation protocols can reduce aspiration incidents and promote safer oral intake. Comprehensive management also includes nutritional support and respiratory care to prevent complications beyond pneumonia, such as malnutrition and respiratory failure.
example of dysphagia in stroke Infographic
 samplerz.com
samplerz.com