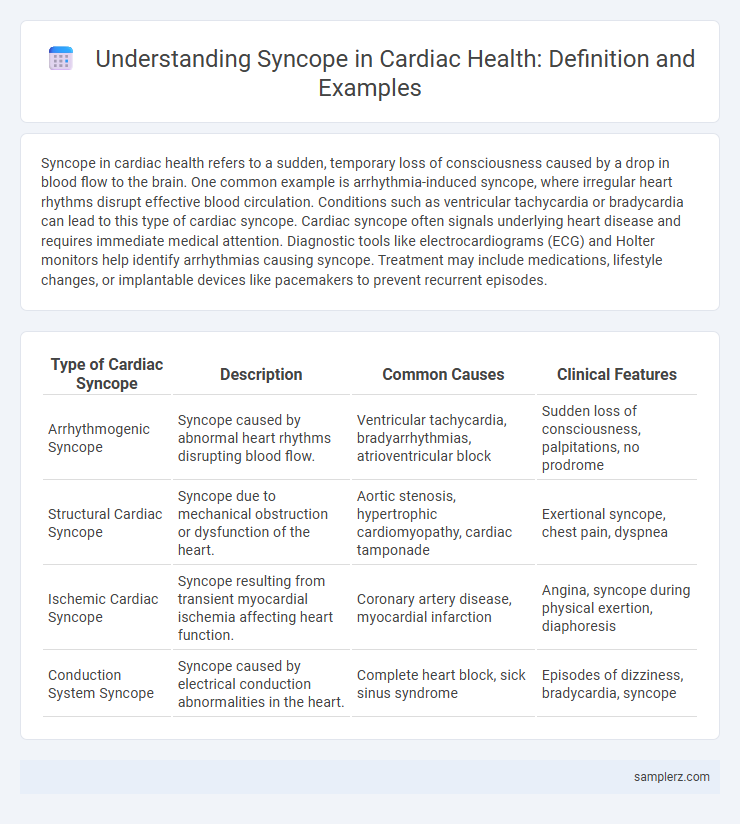
Syncope in cardiac health refers to a sudden, temporary loss of consciousness caused by a drop in blood flow to the brain. One common example is arrhythmia-induced syncope, where irregular heart rhythms disrupt effective blood circulation. Conditions such as ventricular tachycardia or bradycardia can lead to this type of cardiac syncope. Cardiac syncope often signals underlying heart disease and requires immediate medical attention. Diagnostic tools like electrocardiograms (ECG) and Holter monitors help identify arrhythmias causing syncope. Treatment may include medications, lifestyle changes, or implantable devices like pacemakers to prevent recurrent episodes.
Table of Comparison
| Type of Cardiac Syncope | Description | Common Causes | Clinical Features |
|---|---|---|---|
| Arrhythmogenic Syncope | Syncope caused by abnormal heart rhythms disrupting blood flow. | Ventricular tachycardia, bradyarrhythmias, atrioventricular block | Sudden loss of consciousness, palpitations, no prodrome |
| Structural Cardiac Syncope | Syncope due to mechanical obstruction or dysfunction of the heart. | Aortic stenosis, hypertrophic cardiomyopathy, cardiac tamponade | Exertional syncope, chest pain, dyspnea |
| Ischemic Cardiac Syncope | Syncope resulting from transient myocardial ischemia affecting heart function. | Coronary artery disease, myocardial infarction | Angina, syncope during physical exertion, diaphoresis |
| Conduction System Syncope | Syncope caused by electrical conduction abnormalities in the heart. | Complete heart block, sick sinus syndrome | Episodes of dizziness, bradycardia, syncope |
Understanding Cardiac Syncope: Key Concepts
Cardiac syncope is primarily caused by sudden arrhythmias such as ventricular tachycardia or bradycardia, which lead to transient cerebral hypoperfusion and loss of consciousness. Structural heart diseases including cardiomyopathy and aortic stenosis also contribute significantly to syncope episodes by impairing cardiac output. Recognizing these underlying cardiac conditions through diagnostic tools like ECG, Holter monitoring, and echocardiography is essential for accurate diagnosis and effective management.
Common Causes of Cardiac Syncope
Common causes of cardiac syncope include arrhythmias such as ventricular tachycardia and bradycardia, which disrupt normal heart rhythm and reduce cerebral perfusion. Structural heart diseases like aortic stenosis and hypertrophic cardiomyopathy can obstruct blood flow, leading to transient loss of consciousness. Ischemic heart disease often precipitates syncope by impairing myocardial function and triggering abnormal electrical activity.
Classic Clinical Presentations of Cardiac Syncope
Cardiac syncope often presents with sudden loss of consciousness due to transient arrhythmias such as ventricular tachycardia or severe bradycardia, frequently accompanied by palpitations or chest pain. Classic clinical features include abrupt onset without warning, episodes triggered by exertion or emotional stress, and rapid recovery without lingering neurological deficits. These presentations distinguish cardiac syncope from neurogenic causes and necessitate prompt cardiovascular evaluation to prevent sudden cardiac death.
Vasovagal vs. Cardiac Syncope: Key Differences
Vasovagal syncope, often triggered by stress or pain, is characterized by a sudden drop in heart rate and blood pressure leading to brief loss of consciousness and rapid recovery without cardiac abnormalities. Cardiac syncope results from arrhythmias or structural heart diseases, presenting with abrupt loss of consciousness and a higher risk of sudden cardiac death due to compromised cardiac output. Differentiating vasovagal from cardiac syncope relies on patient history, ECG findings, and presence of underlying heart conditions to guide appropriate management and prognosis.
Arrhythmias Leading to Cardiac Syncope
Arrhythmias leading to cardiac syncope commonly include ventricular tachycardia, atrial fibrillation with rapid ventricular response, and bradyarrhythmias such as complete heart block. These abnormal heart rhythms disrupt effective cardiac output, causing transient cerebral hypoperfusion and resulting in syncope. Prompt diagnosis with ECG monitoring and treatment like antiarrhythmic drugs or device implantation is critical to prevent recurrent syncope and sudden cardiac death.
Examples of Structural Heart Diseases Causing Syncope
Structural heart diseases causing syncope include hypertrophic cardiomyopathy, where thickened heart muscle obstructs blood flow, leading to fainting episodes during exertion. Aortic stenosis, characterized by the narrowing of the aortic valve, reduces cardiac output and can trigger syncope, especially with physical activity. Other examples are arrhythmogenic right ventricular cardiomyopathy and severe mitral valve prolapse, both contributing to abnormal heart rhythms and transient loss of consciousness.
Syncope Triggered by Exertion: Warning Signs
Syncope triggered by exertion often indicates underlying cardiac conditions such as hypertrophic cardiomyopathy or arrhythmogenic right ventricular cardiomyopathy, where reduced cardiac output or ventricular arrhythmias impair cerebral perfusion. Warning signs include sudden dizziness, chest pain, palpitations, and shortness of breath during or immediately after physical activity. Prompt recognition of these symptoms is critical to prevent sudden cardiac arrest and guide timely diagnostic evaluation with ECG, echocardiography, or cardiac MRI.
Pediatric and Elderly Cardiac Syncope Cases
Cardiac syncope in pediatric patients often arises from congenital heart defects such as hypertrophic cardiomyopathy and arrhythmogenic right ventricular cardiomyopathy, leading to sudden loss of consciousness due to transient cerebral hypoperfusion. In elderly individuals, cardiac syncope frequently results from ischemic heart disease, aortic stenosis, or atrioventricular conduction blocks, precipitating similar syncopal episodes linked to impaired cardiac output. Early diagnosis and management using electrocardiography, echocardiography, and Holter monitoring are critical in both age groups to prevent recurrent events and reduce mortality risk.
Immediate Assessment Steps for Cardiac Syncope
Evaluate airway, breathing, and circulation immediately in suspected cardiac syncope to ensure patient stability. Obtain a rapid 12-lead ECG to identify arrhythmias or ischemic changes indicative of cardiac causes. Monitor vital signs continuously and prepare for advanced cardiac life support if deterioration occurs.
Long-Term Management of Cardiac Syncope Episodes
Long-term management of cardiac syncope, often caused by arrhythmias like ventricular tachycardia or bradycardia, includes the use of implantable cardioverter-defibrillators (ICDs) and pacemakers to prevent recurrent episodes. Lifestyle modifications, medication adherence such as beta-blockers or antiarrhythmics, and regular cardiac monitoring through Holter devices or event recorders are essential for reducing syncope-related morbidity. Risk stratification via electrophysiological studies helps tailor individualized treatment plans to optimize patient outcomes.
example of syncope in cardiac Infographic
 samplerz.com
samplerz.com