Xerostomia, commonly known as dry mouth, is a frequent side effect of various medications, including antihistamines, antidepressants, and certain antihypertensive drugs. This condition results from reduced saliva production, affecting oral health by increasing the risk of tooth decay, gum disease, and difficulties in speaking and swallowing. Patients experiencing xerostomia often report a persistent dry or sticky feeling in the mouth, which can impact quality of life and nutrition. Clinicians monitor xerostomia closely in patients taking chemotherapy or radiation therapy targeting head and neck cancers. These treatments often damage salivary glands, leading to chronic dry mouth symptoms and increased oral infections. Management strategies include saliva substitutes, good oral hygiene practices, and medications to stimulate saliva production, aiming to alleviate discomfort and prevent oral complications.
Table of Comparison
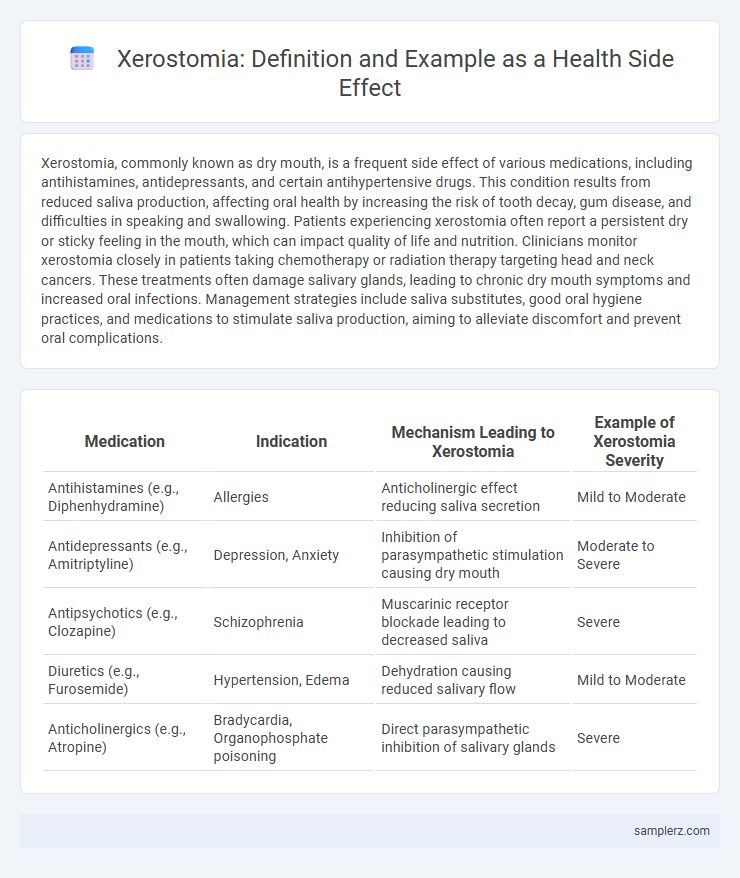
| Medication | Indication | Mechanism Leading to Xerostomia | Example of Xerostomia Severity |
|---|---|---|---|
| Antihistamines (e.g., Diphenhydramine) | Allergies | Anticholinergic effect reducing saliva secretion | Mild to Moderate |
| Antidepressants (e.g., Amitriptyline) | Depression, Anxiety | Inhibition of parasympathetic stimulation causing dry mouth | Moderate to Severe |
| Antipsychotics (e.g., Clozapine) | Schizophrenia | Muscarinic receptor blockade leading to decreased saliva | Severe |
| Diuretics (e.g., Furosemide) | Hypertension, Edema | Dehydration causing reduced salivary flow | Mild to Moderate |
| Anticholinergics (e.g., Atropine) | Bradycardia, Organophosphate poisoning | Direct parasympathetic inhibition of salivary glands | Severe |
Common Medications Leading to Xerostomia
Common medications leading to xerostomia include antihypertensives such as beta-blockers and diuretics, as well as antidepressants like selective serotonin reuptake inhibitors (SSRIs) and tricyclic antidepressants. Anticholinergic drugs used for Parkinson's disease, urinary incontinence, and allergies also frequently cause dry mouth by inhibiting saliva production. Understanding these medication-related risks is crucial for managing xerostomia and preventing associated oral health complications.
Cancer Treatments and Xerostomia Side Effects
Cancer treatments such as radiation therapy and chemotherapy frequently cause xerostomia, a condition characterized by dry mouth due to decreased saliva production. This side effect significantly impacts patients' oral health, increasing the risk of dental caries, oral infections, and difficulty swallowing. Managing xerostomia involves saliva substitutes, hydration, and medications to stimulate saliva flow, improving quality of life for cancer patients.
Xerostomia in Autoimmune Disorders
Xerostomia, commonly known as dry mouth, frequently occurs as a side effect in autoimmune disorders such as Sjogren's syndrome and systemic lupus erythematosus. This condition results from immune-mediated damage to salivary glands, leading to reduced saliva production and increased risk of dental caries and oral infections. Managing xerostomia in autoimmune patients involves saliva substitutes, meticulous oral hygiene, and sometimes immunosuppressive therapy to alleviate gland inflammation.
Antidepressants and Dry Mouth Incidence
Xerostomia, commonly known as dry mouth, is a frequent side effect of antidepressants, particularly selective serotonin reuptake inhibitors (SSRIs) like fluoxetine and sertraline, with incidence rates reported between 20% and 40%. Tricyclic antidepressants (TCAs) such as amitriptyline also exhibit higher xerostomia prevalence due to their strong anticholinergic effects, often exceeding 40% in clinical studies. Management strategies include saliva substitutes, increased hydration, and potential medication adjustments to mitigate the impact on oral health and quality of life.
Xerostomia Associated with Antihypertensive Drugs
Xerostomia, commonly known as dry mouth, frequently occurs as a side effect of antihypertensive drugs such as diuretics, beta-blockers, and calcium channel blockers. These medications reduce saliva production by interfering with autonomic nervous system function, leading to discomfort, increased risk of dental caries, and difficulty in speaking or swallowing. Managing xerostomia in hypertensive patients involves hydration, saliva substitutes, and regular dental check-ups to prevent oral complications.
Chemotherapy-Induced Xerostomia Examples
Chemotherapy-induced xerostomia frequently occurs in patients receiving alkylating agents such as cyclophosphamide and ifosfamide, leading to reduced salivary flow and dry mouth symptoms. Antimetabolites like methotrexate and 5-fluorouracil also contribute to salivary gland hypofunction, increasing the risk of oral infections and mucositis. Targeted therapies including tyrosine kinase inhibitors have been reported to exacerbate xerostomia by damaging salivary gland cells during cancer treatment.
Xerostomia from Antihistamines: Clinical Cases
Xerostomia, a common side effect of antihistamines, manifests as persistent dry mouth due to reduced salivary secretion. Clinical cases highlight patients using first-generation antihistamines like diphenhydramine experiencing severe oral dryness, impacting speech and increasing dental caries risk. Management strategies include saliva substitutes and hydration to alleviate symptoms and improve oral health outcomes.
Xerostomia in Diabetic Patients Taking Medication
Xerostomia, commonly known as dry mouth, frequently occurs as a side effect in diabetic patients taking medications such as antihypertensives, diuretics, and antidiabetic agents like metformin. This condition results from reduced salivary gland function influenced by polypharmacy and the systemic effects of diabetes mellitus. Managing xerostomia in these patients is crucial to prevent complications like oral infections, dental caries, and impaired oral health-related quality of life.
Antipsychotics and Their Link to Dry Mouth
Antipsychotics such as chlorpromazine, haloperidol, and clozapine are frequently associated with xerostomia, a common side effect characterized by persistent dry mouth. This condition results from these medications' anticholinergic properties, which reduce saliva production, potentially leading to difficulties in speaking, chewing, and increased risk of dental caries. Managing xerostomia in patients taking antipsychotics requires regular oral hygiene, hydration, and sometimes saliva substitutes or stimulants to alleviate discomfort and prevent oral complications.
Xerostomia as a Side Effect in Elderly Populations
Xerostomia, commonly known as dry mouth, frequently affects elderly populations as a side effect of medications such as antihypertensives, antidepressants, and diuretics. This condition significantly increases the risk of dental caries, oral infections, and difficulties in swallowing and speaking among older adults. Effective management includes regular hydration, use of saliva substitutes, and periodic dental evaluations to maintain oral health and quality of life.
example of xerostomia in side effect Infographic
 samplerz.com
samplerz.com