Hypoxemia at high altitudes occurs due to reduced atmospheric oxygen pressure, which limits oxygen availability for lung absorption. This condition is commonly observed in mountain climbers and residents living above 2,500 meters, where oxygen saturation in arterial blood can drop significantly below normal levels. Symptoms include shortness of breath, rapid breathing, and decreased physical performance, indicating impaired oxygen delivery to body tissues. Data from studies on altitude hypoxemia demonstrate that oxygen saturation may fall below 85% in individuals ascending rapidly to extreme altitudes, such as above 5,000 meters. This reduction in oxygen levels triggers physiological adaptations like increased red blood cell production and pulmonary vasoconstriction. Monitoring arterial oxygen saturation using pulse oximetry becomes critical for assessing the severity of hypoxemia and guiding medical interventions during high-altitude exposure.
Table of Comparison
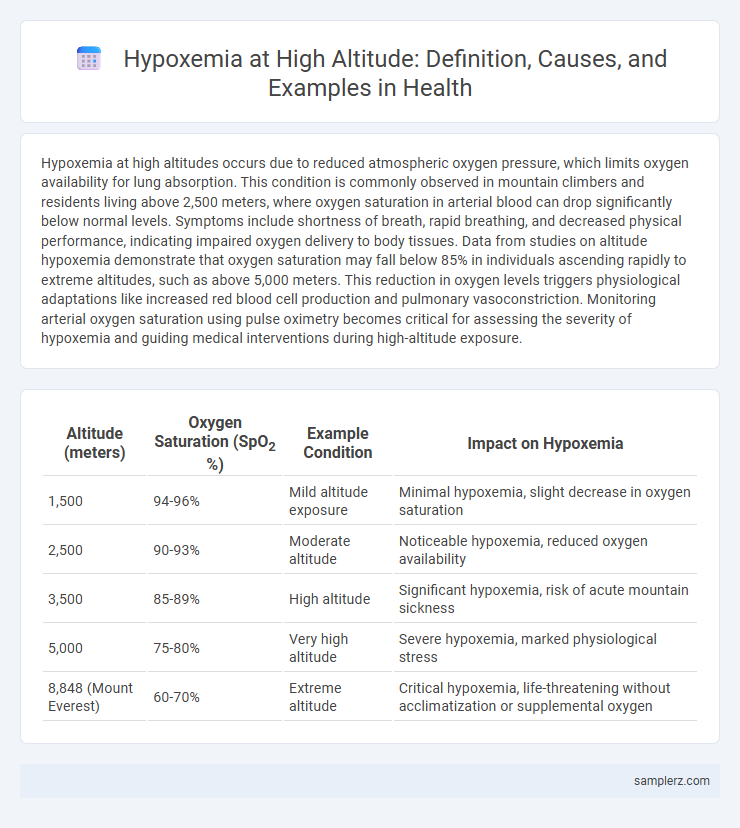
| Altitude (meters) | Oxygen Saturation (SpO2 %) | Example Condition | Impact on Hypoxemia |
|---|---|---|---|
| 1,500 | 94-96% | Mild altitude exposure | Minimal hypoxemia, slight decrease in oxygen saturation |
| 2,500 | 90-93% | Moderate altitude | Noticeable hypoxemia, reduced oxygen availability |
| 3,500 | 85-89% | High altitude | Significant hypoxemia, risk of acute mountain sickness |
| 5,000 | 75-80% | Very high altitude | Severe hypoxemia, marked physiological stress |
| 8,848 (Mount Everest) | 60-70% | Extreme altitude | Critical hypoxemia, life-threatening without acclimatization or supplemental oxygen |
Understanding Hypoxemia at High Altitudes
Hypoxemia at high altitudes occurs due to reduced atmospheric oxygen pressure, leading to lower oxygen saturation in the blood. This condition commonly affects climbers and residents above 8,000 feet, causing symptoms like shortness of breath, dizziness, and fatigue. Understanding altitude hypoxemia is critical for preventing acute mountain sickness and ensuring proper acclimatization strategies.
Physiological Effects of Altitude-Induced Hypoxemia
Altitude-induced hypoxemia occurs when reduced atmospheric oxygen pressure at high elevations leads to decreased arterial oxygen saturation, causing tissue hypoxia. This condition triggers physiological responses such as increased respiratory rate, elevated heart rate, and enhanced erythropoiesis to improve oxygen delivery. Prolonged exposure can result in altitude sickness, pulmonary hypertension, and impaired cognitive and physical performance.
Common Causes of Hypoxemia in Mountain Environments
Hypoxemia at high altitudes commonly results from reduced atmospheric oxygen pressure, leading to decreased arterial oxygen saturation. Mountain environments also cause hypoxemia through factors like hypoventilation due to acclimatization delays and pulmonary edema induced by extreme altitude exposure. These physiological stressors collectively reduce oxygen supply to tissues, requiring careful management and acclimatization strategies.
Recognizing Symptoms of Altitude Hypoxemia
Symptoms of altitude hypoxemia include headache, dizziness, shortness of breath, and fatigue, often occurring above 8,000 feet (2,400 meters). Recognizing tachycardia, cyanosis, and confusion is crucial for early diagnosis, as these indicate decreased oxygen saturation in the blood. Immediate descent and supplemental oxygen administration are critical interventions to prevent progression to high-altitude pulmonary edema or cerebral edema.
Real-Life Case Studies: Hypoxemia During Mountaineering
A notable case of hypoxemia during mountaineering occurred on Mount Everest, where climbers frequently experience oxygen saturation levels dropping below 80% at elevations above 8,000 meters. Research on Sherpa guides demonstrated their remarkable adaptation to high altitude, maintaining higher arterial oxygen content compared to lowland climbers, which reduces the severity of hypoxemia. These real-life instances highlight the critical importance of acclimatization and supplemental oxygen in preventing severe hypoxemia and altitude sickness at extreme elevations.
Risk Factors for Developing Hypoxemia at Elevation
Exposure to high altitudes above 8,000 feet significantly increases the risk of hypoxemia due to reduced atmospheric oxygen pressure. Individuals with pre-existing respiratory conditions, such as chronic obstructive pulmonary disease (COPD) or asthma, and those with anemia or cardiovascular diseases are particularly vulnerable. Rapid ascent without adequate acclimatization exacerbates oxygen deprivation, elevating the risk of acute mountain sickness and severe hypoxemia.
Hypoxemia vs. Hypoxia: Differences at Altitude
Hypoxemia at high altitudes results from reduced atmospheric oxygen pressure, leading to decreased oxygen saturation in the blood. Unlike hypoxia, which refers to insufficient oxygen at the tissue level, hypoxemia specifically denotes low arterial oxygen levels measured by pulse oximetry or arterial blood gases. Understanding the distinction is critical for managing altitude sickness and preventing complications such as acute mountain sickness or high-altitude pulmonary edema.
Prevention Strategies for Altitude Hypoxemia
Preventing altitude hypoxemia involves gradual ascent to allow acclimatization, minimizing the risk of reduced oxygen saturation at high elevations. Using supplemental oxygen during climbs above 2,500 meters significantly improves arterial oxygen levels. Maintaining hydration, avoiding alcohol, and considering medications like acetazolamide further support respiratory function and enhance acclimatization.
Emergency Response and Management of Hypoxemia in Altitude
Hypoxemia at high altitude commonly occurs due to decreased barometric pressure leading to reduced oxygen saturation in the blood, necessitating prompt emergency response. Immediate administration of supplemental oxygen and descent to lower altitudes constitute primary management strategies to prevent severe complications such as high-altitude pulmonary edema (HAPE) and cerebral edema (HACE). Continuous monitoring of oxygen saturation and rapid evacuation protocols are critical components in managing altitude-induced hypoxemia effectively.
Long-Term Adaptation to Hypoxemic Conditions at High Altitude
Long-term adaptation to hypoxemia at high altitude involves physiological changes such as increased red blood cell production, enhanced oxygen affinity of hemoglobin, and angiogenesis to improve tissue oxygenation. Populations living above 2,500 meters, like those in the Andes or Himalayas, exhibit these adaptations to mitigate chronic low oxygen saturation levels typically below 90%. These mechanisms collectively maintain cellular metabolism and prevent complications linked to sustained hypoxemia in extreme altitudes.
example of hypoxemia in altitude Infographic
 samplerz.com
samplerz.com