Psychoneuroimmunology studies the interaction between the nervous system, immune system, and psychological processes. In the context of stress, this field examines how chronic stress triggers the release of cortisol, a hormone that suppresses immune function. Elevated cortisol levels can decrease the body's ability to fight infections, resulting in increased susceptibility to illnesses. Research in psychoneuroimmunology demonstrates that psychological stress influences cytokine production, which regulates inflammation and immune response. Stress-induced changes in the hypothalamic-pituitary-adrenal (HPA) axis impact immune cell activity, leading to altered immune defense. Understanding these connections helps in developing interventions to reduce stress-related immune dysfunction and improve overall health outcomes.
Table of Comparison
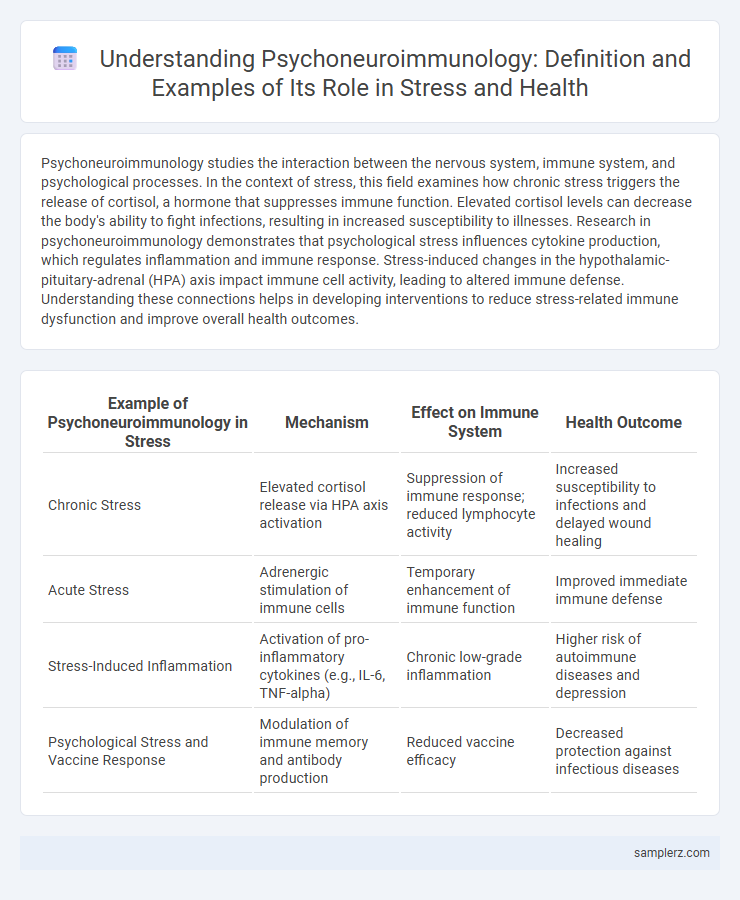
| Example of Psychoneuroimmunology in Stress | Mechanism | Effect on Immune System | Health Outcome |
|---|---|---|---|
| Chronic Stress | Elevated cortisol release via HPA axis activation | Suppression of immune response; reduced lymphocyte activity | Increased susceptibility to infections and delayed wound healing |
| Acute Stress | Adrenergic stimulation of immune cells | Temporary enhancement of immune function | Improved immediate immune defense |
| Stress-Induced Inflammation | Activation of pro-inflammatory cytokines (e.g., IL-6, TNF-alpha) | Chronic low-grade inflammation | Higher risk of autoimmune diseases and depression |
| Psychological Stress and Vaccine Response | Modulation of immune memory and antibody production | Reduced vaccine efficacy | Decreased protection against infectious diseases |
Introduction to Psychoneuroimmunology and Stress
Psychoneuroimmunology examines the interaction between the nervous system, immune response, and psychological processes during stress exposure. Stress activates the hypothalamic-pituitary-adrenal (HPA) axis, releasing cortisol, which suppresses immune function and increases vulnerability to infections. Chronic stress-induced immune dysregulation has been linked to inflammation-related diseases, demonstrating the vital role of psychoneuroimmunology in understanding stress-related health outcomes.
The Mind-Body Connection in Stress Responses
Psychoneuroimmunology demonstrates how chronic stress triggers the hypothalamic-pituitary-adrenal (HPA) axis, resulting in increased cortisol production that suppresses immune function. Studies reveal that elevated cortisol levels reduce lymphocyte activity, impairing the body's ability to fight infections and increasing vulnerability to illness. This mind-body connection highlights the critical role of psychological stress in modulating immune responses, influencing overall health and disease susceptibility.
How Stress Alters Immune System Function
Stress triggers the release of cortisol, a hormone that suppresses immune cell activity and reduces the production of cytokines essential for immune response. Chronic stress leads to prolonged elevation of cortisol levels, impairing the function of T-cells and decreasing antibody formation, which increases susceptibility to infections. Psychoneuroimmunology research demonstrates how neural and endocrine responses to stress disrupt the balance of immune mechanisms.
Neurotransmitters and Hormonal Changes During Stress
Stress triggers the release of neurotransmitters such as norepinephrine and dopamine, which modulate brain activity and influence immune responses. Concurrent hormonal changes involve elevated cortisol levels from the adrenal glands that suppress immune function and promote inflammation. Psychoneuroimmunology studies reveal these interactions between the nervous, endocrine, and immune systems, highlighting their complex role in stress-related health outcomes.
Chronic Stress and Increased Susceptibility to Illness
Chronic stress triggers prolonged activation of the hypothalamic-pituitary-adrenal (HPA) axis, leading to elevated cortisol levels that suppress immune function. This immunosuppression increases vulnerability to infections such as the common cold and influenza. Research in psychoneuroimmunology demonstrates that persistent psychological stress impairs cytokine production, reducing the body's ability to mount effective immune responses.
Real-World Case Studies: Stress Impacting Immunity
Chronic stress in caregivers of Alzheimer's patients has been linked to significantly reduced immune function, as evidenced by lower natural killer cell activity and increased susceptibility to infectious diseases. A study published in Psychosomatic Medicine showed that stressed individuals exhibited delayed wound healing due to impaired inflammatory responses. These real-world case studies highlight the critical role of psychoneuroimmunology in understanding how psychological stress directly affects immune resilience and overall health outcomes.
Psychological Interventions Improving Immune Response
Psychoneuroimmunology research reveals that cognitive-behavioral therapy (CBT) effectively reduces cortisol levels, thereby enhancing immune cell function in individuals experiencing chronic stress. Studies demonstrate that mindfulness-based stress reduction (MBSR) strengthens natural killer cell activity, promoting improved immune response. These psychological interventions modulate neuroendocrine pathways, optimizing immunological health and reducing inflammation markers.
Role of Social Support in Modulating Stress Effects
Social support significantly modulates stress effects by enhancing immune function and reducing inflammation through psychoneuroimmunology pathways. Research shows that individuals with strong social networks exhibit lower cortisol levels and improved cytokine profiles, indicating better stress regulation. This interaction highlights the critical role of social bonds in buffering the negative impacts of chronic stress on health outcomes.
Mindfulness and Stress Reduction: Immune Benefits
Mindfulness-Based Stress Reduction (MBSR) techniques have demonstrated significant improvements in immune function by reducing stress-related inflammation and enhancing antibody responses. Research in psychoneuroimmunology reveals that consistent mindfulness practice lowers cortisol levels, which helps modulate immune system activity and improve resistance to infections. These immune benefits highlight the critical role of mind-body interventions in managing stress and promoting overall health.
Future Directions in Psychoneuroimmunology Research
Future directions in psychoneuroimmunology research emphasize exploring molecular mechanisms linking stress to immune system dysregulation, particularly through neuroendocrine pathways involving cortisol and cytokine imbalances. Advanced neuroimaging combined with immunological biomarkers promises to unravel how chronic stress impacts brain-immune communication, potentially leading to novel interventions for autoimmune and psychiatric disorders. Precision medicine approaches integrating genetic, epigenetic, and environmental data aim to develop targeted therapies that mitigate stress-induced immune dysfunction and improve overall health outcomes.
example of psychoneuroimmunology in stress Infographic
 samplerz.com
samplerz.com