Hemoptysis is a common symptom in patients with tuberculosis, characterized by coughing up blood from the respiratory tract. This condition occurs due to the erosion of blood vessels in the lungs caused by the tuberculous infection. Clinical data reveal that hemoptysis severity varies from mild streaks of blood to significant bleeding, posing a serious risk for affected individuals. In tuberculosis cases, hemoptysis often indicates advanced disease or lung tissue destruction. Diagnostic imaging, such as chest X-rays, frequently shows cavitary lesions that correlate with bleeding sites. Effective management includes anti-tubercular therapy combined with interventions to control bleeding, critical for improving patient outcomes and preventing complications.
Table of Comparison
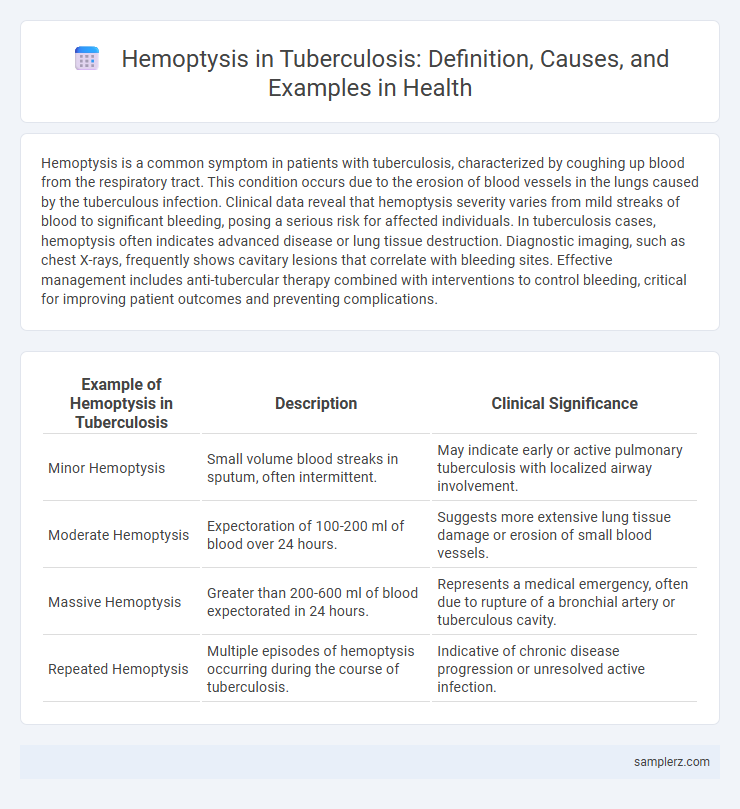
| Example of Hemoptysis in Tuberculosis | Description | Clinical Significance |
|---|---|---|
| Minor Hemoptysis | Small volume blood streaks in sputum, often intermittent. | May indicate early or active pulmonary tuberculosis with localized airway involvement. |
| Moderate Hemoptysis | Expectoration of 100-200 ml of blood over 24 hours. | Suggests more extensive lung tissue damage or erosion of small blood vessels. |
| Massive Hemoptysis | Greater than 200-600 ml of blood expectorated in 24 hours. | Represents a medical emergency, often due to rupture of a bronchial artery or tuberculous cavity. |
| Repeated Hemoptysis | Multiple episodes of hemoptysis occurring during the course of tuberculosis. | Indicative of chronic disease progression or unresolved active infection. |
Understanding Hemoptysis in Tuberculosis
Hemoptysis in tuberculosis occurs due to lung tissue destruction and erosion of blood vessels caused by Mycobacterium tuberculosis infection. Patients may present with varying amounts of blood-streaked sputum or massive coughing of blood, posing significant risk for airway obstruction or hemorrhagic shock. Early diagnosis and management, including sputum analysis and chest imaging, are crucial to prevent severe complications and improve patient outcomes.
Common Causes of Hemoptysis in TB Patients
Hemoptysis in tuberculosis patients commonly arises due to cavitary lesions eroding bronchial arteries, leading to bleeding. Bronchiectasis and granulomatous inflammation also contribute to vascular damage causing persistent or massive hemoptysis. Identifying and managing these complications is critical to prevent life-threatening hemorrhage in TB cases.
Clinical Presentation: How Hemoptysis Manifests in TB
Hemoptysis in tuberculosis typically presents as coughing up small to moderate amounts of bright red blood, often accompanied by persistent cough and chest pain. In advanced cases, significant hemoptysis indicates cavitary lung lesions causing erosion of blood vessels within the pulmonary parenchyma. Clinical evaluation often reveals associated symptoms such as weight loss, night sweats, and fever, confirming active pulmonary TB infection.
Pathophysiology of Hemoptysis in Tuberculosis
Hemoptysis in tuberculosis results from the erosion of pulmonary blood vessels due to granulomatous inflammation and caseous necrosis within lung tissues. The formation of cavitary lesions disrupts bronchial arteries, leading to vessel rupture and bleeding into the airways. Chronic inflammatory processes promote neovascularization, increasing vascular fragility and risk of hemorrhage in affected lung segments.
Case Examples: Hemoptysis Episodes in Pulmonary TB
In pulmonary tuberculosis, hemoptysis commonly presents as recurrent episodes of coughing up blood, ranging from mild streaks to massive hemorrhage. Case studies reveal that hemoptysis severity correlates with cavitary lesions and bronchial artery erosion caused by Mycobacterium tuberculosis infection. Effective management requires timely diagnosis using sputum microscopy and chest radiography to prevent life-threatening complications.
Diagnostic Approaches for Hemoptysis in TB
Diagnosis of hemoptysis in tuberculosis primarily involves chest X-rays and sputum analysis to identify Mycobacterium tuberculosis. Computed tomography (CT) scans provide detailed imaging to assess the extent of lung cavitation and vascular involvement. Bronchoscopy is utilized for direct visualization and biopsy when sputum tests are inconclusive or massive hemoptysis is present.
Complications of Hemoptysis During Tuberculosis Infection
Hemoptysis in tuberculosis often results from the erosion of blood vessels within cavitary lung lesions, leading to potentially life-threatening bleeding. Complications include severe airway obstruction, aspiration pneumonia, and massive hemorrhage that may require urgent bronchial artery embolization or surgical intervention. Timely diagnosis and management are critical to prevent respiratory failure and reduce mortality associated with tuberculosis-related hemoptysis.
Management Strategies for TB-Associated Hemoptysis
Management strategies for TB-associated hemoptysis involve prompt assessment of bleeding severity and stability, with initial measures including airway protection and oxygen supplementation. Medical treatment prioritizes anti-tubercular therapy combined with supportive care such as hemostatic agents and blood transfusion in severe cases. Interventional procedures like bronchial artery embolization and surgical resection remain critical options for persistent or life-threatening hemorrhage in tuberculosis patients.
Prognosis: Outcomes of Hemoptysis in TB Cases
Hemoptysis in tuberculosis patients varies widely in prognosis depending on the severity and extent of pulmonary involvement. Mild hemoptysis often resolves with standard anti-tubercular therapy, while massive hemoptysis can lead to life-threatening respiratory failure or require interventional procedures like bronchial artery embolization. Early detection and appropriate management significantly improve survival rates and reduce complications in TB-related hemoptysis cases.
Preventive Measures for Hemoptysis in Tuberculosis Patients
Effective preventive measures for hemoptysis in tuberculosis patients include early diagnosis and strict adherence to anti-tubercular therapy to reduce lung tissue damage. Regular monitoring through sputum examination and chest X-rays helps detect disease progression and potential bleeding risks. Maintaining proper nutrition and avoiding smoking also support lung health and minimize the risk of hemoptysis.
example of hemoptysis in tuberculosis Infographic
 samplerz.com
samplerz.com