Dysphagia in otolaryngology commonly presents as difficulty swallowing due to structural or neurological issues in the throat or esophagus. One example is oropharyngeal dysphagia caused by a tumor in the hypopharynx that obstructs the passage of food. Another case involves vocal cord paralysis, which impairs the swallowing mechanism and increases the risk of aspiration. Data from clinical studies indicate that oropharyngeal dysphagia affects approximately 15% of patients seen in otolaryngology clinics. Imaging techniques such as videofluoroscopic swallow studies provide detailed assessments of swallowing function and help identify the underlying pathology. Early detection and targeted therapy improve outcomes by reducing complications like pneumonia and malnutrition.
Table of Comparison
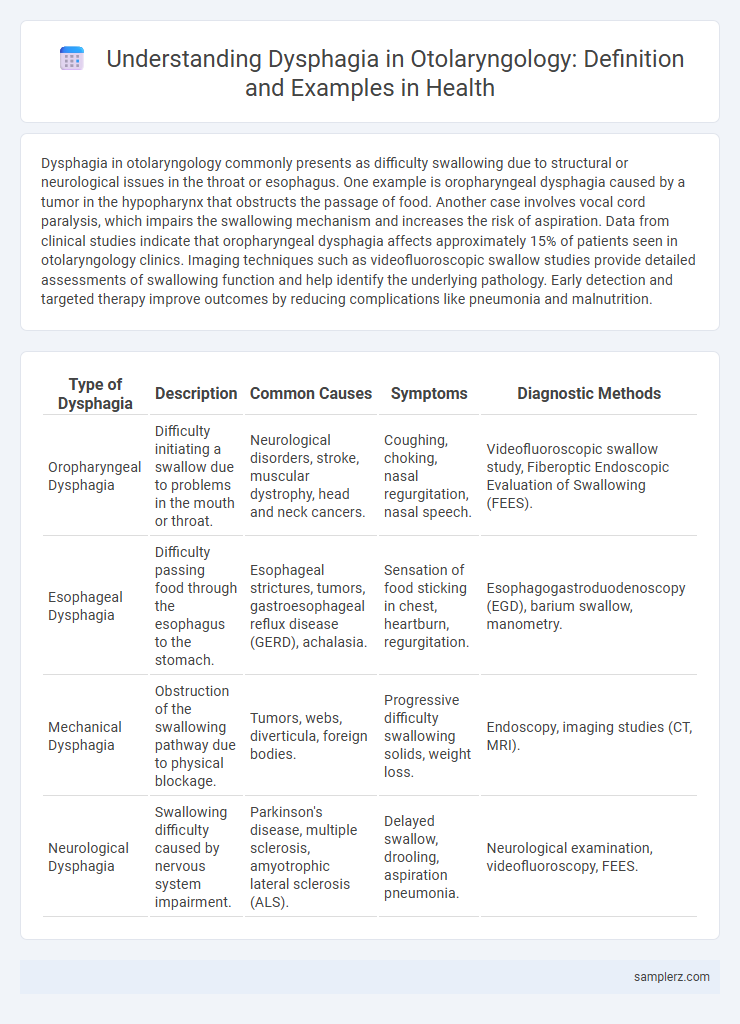
| Type of Dysphagia | Description | Common Causes | Symptoms | Diagnostic Methods |
|---|---|---|---|---|
| Oropharyngeal Dysphagia | Difficulty initiating a swallow due to problems in the mouth or throat. | Neurological disorders, stroke, muscular dystrophy, head and neck cancers. | Coughing, choking, nasal regurgitation, nasal speech. | Videofluoroscopic swallow study, Fiberoptic Endoscopic Evaluation of Swallowing (FEES). |
| Esophageal Dysphagia | Difficulty passing food through the esophagus to the stomach. | Esophageal strictures, tumors, gastroesophageal reflux disease (GERD), achalasia. | Sensation of food sticking in chest, heartburn, regurgitation. | Esophagogastroduodenoscopy (EGD), barium swallow, manometry. |
| Mechanical Dysphagia | Obstruction of the swallowing pathway due to physical blockage. | Tumors, webs, diverticula, foreign bodies. | Progressive difficulty swallowing solids, weight loss. | Endoscopy, imaging studies (CT, MRI). |
| Neurological Dysphagia | Swallowing difficulty caused by nervous system impairment. | Parkinson's disease, multiple sclerosis, amyotrophic lateral sclerosis (ALS). | Delayed swallow, drooling, aspiration pneumonia. | Neurological examination, videofluoroscopy, FEES. |
Common Oropharyngeal Causes of Dysphagia
Common oropharyngeal causes of dysphagia in otolaryngology include neuromuscular disorders such as stroke, Parkinson's disease, and myasthenia gravis, which impair the coordination of swallowing muscles. Structural abnormalities like Zenker's diverticulum and pharyngeal tumors also contribute to swallowing difficulties by obstructing the oropharyngeal pathway. These conditions often manifest as coughing, choking, or nasal regurgitation during swallowing, necessitating thorough clinical evaluation and targeted therapeutic interventions.
Esophageal Dysphagia: Key Otolaryngology Cases
Esophageal dysphagia in otolaryngology often presents through cases involving structural abnormalities such as strictures, rings, or tumors obstructing the esophagus. Diagnostic evaluation frequently includes endoscopy and barium swallow studies to identify causes like esophageal motility disorders or malignancies. Management strategies range from dilation procedures to surgical resection depending on the underlying pathology and severity of symptoms.
Neurological Disorders Presenting with Dysphagia
Neurological disorders such as stroke, Parkinson's disease, and multiple sclerosis frequently present with dysphagia due to impaired coordination and muscle weakness affecting the swallowing mechanism. In otolaryngology, these conditions require comprehensive evaluation including videofluoroscopic swallow studies to assess the severity and specific phase of swallowing disruption. Early diagnosis and targeted rehabilitation strategies improve patient outcomes by reducing aspiration risk and enhancing nutritional status.
Dysphagia Related to Head and Neck Tumors
Dysphagia related to head and neck tumors frequently occurs due to obstruction or infiltration of the pharynx, larynx, or esophagus by malignant masses. Patients often present with progressive difficulty swallowing, pain, and weight loss, signaling advanced tumor involvement affecting speech and airway protection. Early detection through endoscopic examination and imaging is crucial for timely intervention and improved prognosis in otolaryngology practice.
Post-Surgical Dysphagia in Otolaryngology
Post-surgical dysphagia in otolaryngology commonly occurs after procedures such as laryngectomy, thyroidectomy, or cervical spine surgery, leading to impaired swallowing function due to structural and neurological changes. This condition often results from nerve injury, edema, or scarring affecting the pharyngeal muscles and cranial nerves involved in swallowing. Early diagnosis and targeted rehabilitation, including swallowing therapy and dietary modifications, are crucial for improving patient outcomes and preventing complications like aspiration pneumonia.
Pediatric Dysphagia: ENT Perspectives
Pediatric dysphagia, a common concern in otolaryngology, involves difficulty swallowing in children due to anatomical or neurological abnormalities. Conditions such as cleft palate, laryngeal clefts, and vocal cord paralysis significantly impact swallowing function and require targeted evaluation by ENT specialists. Early diagnosis and multidisciplinary management optimize feeding safety and prevent aspiration pneumonia in affected pediatric patients.
Inflammatory Conditions Causing Dysphagia
Inflammatory conditions such as esophagitis and pharyngitis frequently cause dysphagia by swelling and irritation of the mucosal lining in the throat and esophagus. In otolaryngology, viral infections like herpes simplex virus and bacterial infections such as Streptococcus pyogenes are common triggers of inflammation leading to painful or difficult swallowing. Effective diagnosis often involves endoscopic examination and biopsy to differentiate between infectious and autoimmune etiologies, including eosinophilic esophagitis.
Iatrogenic Dysphagia: Complications of Otolaryngologic Procedures
Iatrogenic dysphagia is a common complication following otolaryngologic procedures such as thyroidectomy, cervical spine surgery, and head and neck radiotherapy. Damage to the recurrent laryngeal nerve or pharyngeal muscles during these interventions can lead to impaired swallowing and aspiration risks. Early diagnosis with videofluoroscopic swallow studies and targeted rehabilitation are essential to improve patient outcomes and reduce morbidity.
Structural Abnormalities Leading to Swallowing Difficulties
Structural abnormalities such as esophageal strictures, Zenker's diverticulum, and cervical osteophytes commonly cause dysphagia in otolaryngology by obstructing or altering the swallowing pathway. These conditions disrupt normal bolus transit, leading to symptoms like food sticking or aspiration risk. Precise diagnosis through endoscopy or imaging is critical for targeted treatment and preventing complications.
Diagnostic Approaches to Dysphagia in Otolaryngology
Diagnostic approaches to dysphagia in otolaryngology include videofluoroscopic swallow studies (VFSS) and fiberoptic endoscopic evaluation of swallowing (FEES), which provide detailed visualization of swallowing mechanics. High-resolution manometry offers precise assessment of pharyngeal and esophageal pressures, aiding in identifying motility disorders contributing to dysphagia. Comprehensive clinical evaluation combined with imaging techniques ensures accurate differentiation between oropharyngeal and esophageal dysphagia, guiding targeted therapeutic interventions.
example of dysphagia in otolaryngology Infographic
 samplerz.com
samplerz.com