Comorbidity in a patient refers to the presence of two or more chronic diseases or conditions occurring simultaneously. A common example of comorbidity is a patient suffering from type 2 diabetes alongside hypertension. These conditions often share risk factors such as obesity and poor diet, compounding the patient's overall health risks. Patients with comorbid conditions require integrated treatment plans to address multiple health issues concurrently. Managing a patient with both diabetes and hypertension involves regular monitoring of blood glucose levels and blood pressure. Effective comorbidity management can reduce hospital admissions and improve quality of life for patients with complex health profiles.
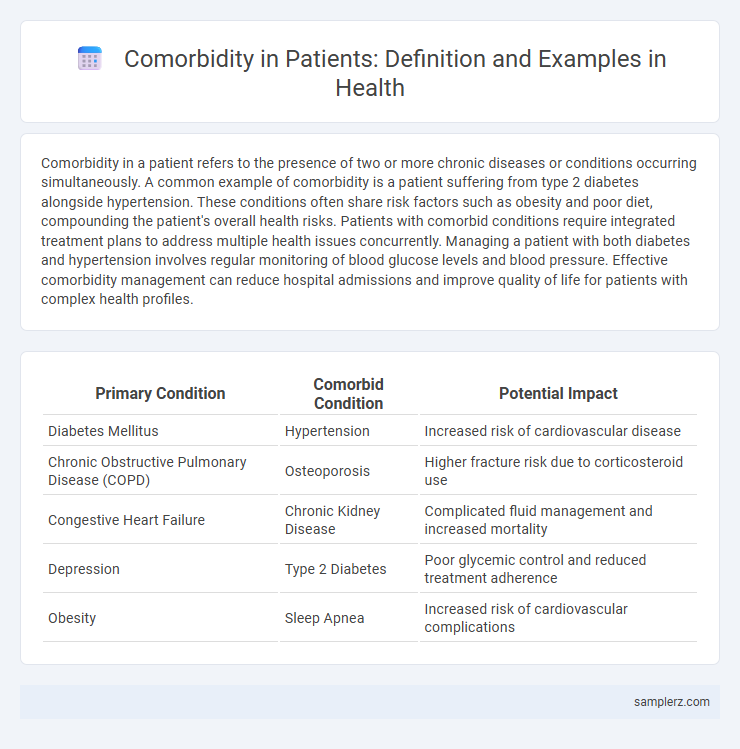
Table of Comparison
| Primary Condition | Comorbid Condition | Potential Impact |
|---|---|---|
| Diabetes Mellitus | Hypertension | Increased risk of cardiovascular disease |
| Chronic Obstructive Pulmonary Disease (COPD) | Osteoporosis | Higher fracture risk due to corticosteroid use |
| Congestive Heart Failure | Chronic Kidney Disease | Complicated fluid management and increased mortality |
| Depression | Type 2 Diabetes | Poor glycemic control and reduced treatment adherence |
| Obesity | Sleep Apnea | Increased risk of cardiovascular complications |
Understanding Comorbidity: Definition and Significance
Comorbidity refers to the simultaneous presence of two or more chronic diseases or conditions in a patient, such as diabetes and hypertension occurring together. Understanding comorbidity is essential for accurate diagnosis, effective treatment planning, and predicting patient outcomes. It highlights the complex interplay between multiple health issues that can exacerbate symptoms and complicate clinical management.
Common Chronic Disease Comorbidities
Diabetes mellitus often coexists with hypertension, creating a complex comorbidity that increases the risk of cardiovascular disease. Chronic obstructive pulmonary disease (COPD) frequently occurs alongside heart failure, exacerbating respiratory and cardiac symptoms. These common chronic disease comorbidities require integrated management to improve patient outcomes and reduce healthcare costs.
Diabetes: Frequent Comorbid Conditions
Diabetes frequently coexists with hypertension, cardiovascular disease, and chronic kidney disease, significantly increasing patient morbidity and healthcare complexity. Diabetic neuropathy and retinopathy often occur alongside, leading to severe complications if not managed properly. Effective treatment plans must address these common comorbid conditions to improve patient outcomes and reduce hospitalizations.
Hypertension and Its Associated Comorbidities
Hypertension frequently coexists with comorbidities such as type 2 diabetes mellitus, chronic kidney disease, and cardiovascular disorders including coronary artery disease and heart failure. These associated conditions amplify the risk of adverse health outcomes, complicate treatment regimens, and increase healthcare utilization. Effective management of hypertension requires integrated care strategies addressing both blood pressure control and the specific comorbid conditions to reduce overall morbidity and mortality.
Mental Health Disorders and Comorbid Physical Illnesses
Patients with depression often experience comorbid physical illnesses such as cardiovascular disease and diabetes, which complicate treatment outcomes and increase mortality risk. Anxiety disorders frequently coexist with chronic respiratory conditions like asthma, exacerbating symptoms and reducing quality of life. Effective management requires integrated care addressing both mental health disorders and associated physical illnesses to improve overall patient prognosis.
Obesity-Related Comorbidities in Patients
Obesity-related comorbidities in patients commonly include type 2 diabetes mellitus, hypertension, and obstructive sleep apnea, significantly increasing the risk for cardiovascular diseases. These conditions often coexist, exacerbating metabolic dysfunction and leading to complications such as chronic kidney disease and nonalcoholic fatty liver disease. Effective management requires addressing obesity through multidisciplinary approaches including lifestyle modification, pharmacotherapy, and in some cases, bariatric surgery.
Cardiovascular Disease Comorbidity Examples
Patients with cardiovascular disease often present comorbidities such as hypertension, diabetes mellitus, and chronic kidney disease, which complicate treatment and worsen prognosis. The coexistence of atrial fibrillation and heart failure is a frequent example, increasing the risk of stroke and mortality. Managing these comorbid conditions requires a multidisciplinary approach to optimize cardiovascular outcomes and reduce hospitalizations.
Comorbidities in Elderly Patients
Elderly patients often experience comorbidities such as hypertension, type 2 diabetes, and osteoarthritis, which complicate treatment plans and increase hospitalization risks. The presence of chronic kidney disease alongside congestive heart failure is common, leading to decreased functional status and higher mortality rates. Effective management requires integrated care approaches targeting multiple conditions simultaneously to improve health outcomes in this demographic.
Impact of Comorbidity on Patient Outcomes
Comorbidity, such as diabetes combined with hypertension, significantly worsens patient outcomes by increasing the risk of cardiovascular events and complicating treatment protocols. Studies indicate that patients with multiple chronic conditions experience higher rates of hospitalization and mortality compared to those with a single illness. Effective management of comorbidities requires integrated care approaches to reduce adverse health impacts and improve overall patient prognosis.
Approaches to Managing Multiple Comorbidities
Managing multiple comorbidities, such as diabetes coexisting with hypertension and chronic kidney disease, requires integrated care plans that prioritize medication reconciliation and patient-centered goal setting. Utilizing multidisciplinary teams, including primary care physicians, specialists, and pharmacists, enhances coordination and reduces treatment conflicts. Implementing personalized health monitoring and lifestyle interventions further improves patient outcomes and quality of life.
example of comorbidity in patient Infographic
 samplerz.com
samplerz.com