Polypharmacy in elderly patients often involves the concurrent use of multiple medications to manage chronic conditions such as hypertension, diabetes, and arthritis. A typical case may include an elderly individual prescribed antihypertensives, insulin or oral hypoglycemics, statins, and nonsteroidal anti-inflammatory drugs (NSAIDs). This combination exemplifies polypharmacy by addressing distinct health issues but also increases the risk of drug interactions and adverse effects. Data from healthcare studies indicate that approximately 40% of elderly patients take five or more medications daily, highlighting the prevalence of polypharmacy in this demographic. The complexity of managing multiple prescriptions necessitates careful monitoring by healthcare providers to prevent complications like falls, cognitive decline, or hospital readmissions. Effective medication review and patient education remain critical in optimizing outcomes for elderly patients experiencing polypharmacy.
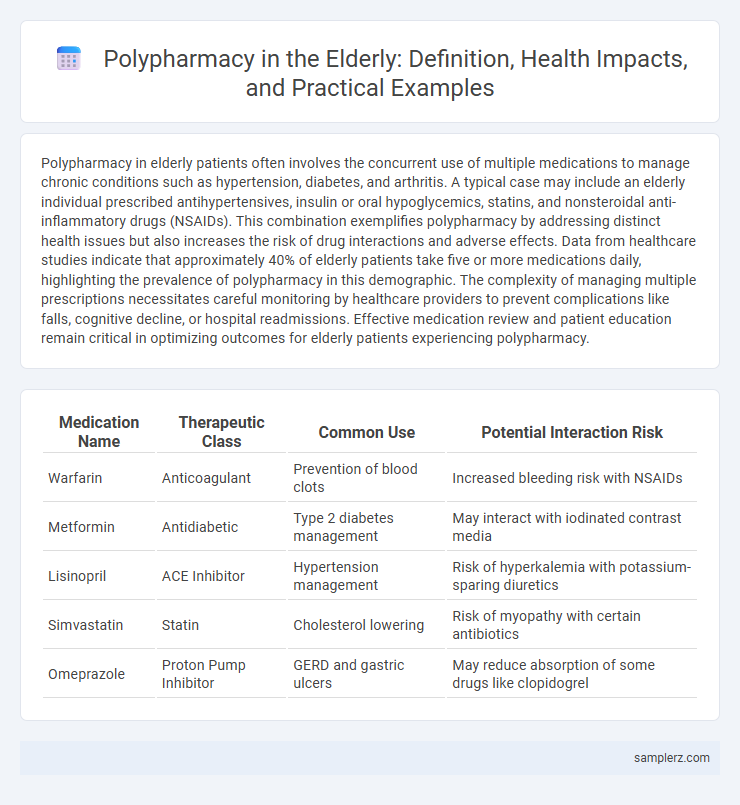
Table of Comparison
| Medication Name | Therapeutic Class | Common Use | Potential Interaction Risk |
|---|---|---|---|
| Warfarin | Anticoagulant | Prevention of blood clots | Increased bleeding risk with NSAIDs |
| Metformin | Antidiabetic | Type 2 diabetes management | May interact with iodinated contrast media |
| Lisinopril | ACE Inhibitor | Hypertension management | Risk of hyperkalemia with potassium-sparing diuretics |
| Simvastatin | Statin | Cholesterol lowering | Risk of myopathy with certain antibiotics |
| Omeprazole | Proton Pump Inhibitor | GERD and gastric ulcers | May reduce absorption of some drugs like clopidogrel |
Understanding Polypharmacy in the Elderly
Polypharmacy in the elderly often involves the simultaneous use of multiple medications such as antihypertensives, antidiabetics, and anticoagulants to manage chronic conditions like hypertension, diabetes, and atrial fibrillation. This complex medication regimen increases the risk of adverse drug reactions, drug interactions, and medication non-adherence. Understanding polypharmacy is essential to optimize therapeutic outcomes and minimize potential harm through regular medication reviews and personalized care plans.
Common Drug Combinations in Older Adults
Common drug combinations in older adults often include antihypertensives paired with diuretics, antidiabetics combined with statins, and the simultaneous use of benzodiazepines alongside opioid analgesics. These combinations increase the risk of adverse drug interactions and complicate medication management, leading to higher rates of hospitalizations in elderly populations. Careful review and monitoring by healthcare providers are essential to minimize polypharmacy-related risks and optimize therapeutic outcomes.
Risks of Polypharmacy Among Senior Patients
Polypharmacy in elderly patients, often defined as the concurrent use of five or more medications, significantly increases the risk of adverse drug reactions, medication non-adherence, and drug-drug interactions. Seniors with multiple chronic conditions such as hypertension, diabetes, and arthritis are particularly vulnerable to these risks, which can lead to falls, cognitive impairment, hospitalizations, and higher mortality rates. Careful medication review and management strategies are essential to minimize these dangers and improve health outcomes among older adults.
Case Studies: Polypharmacy Scenarios in Elderly Care
Elderly patients with multiple chronic conditions often experience polypharmacy, as demonstrated in case studies where individuals manage diabetes, hypertension, and arthritis simultaneously, resulting in the use of five or more medications. These scenarios reveal the increased risk of adverse drug interactions and medication non-adherence, complicating treatment outcomes and highlighting the need for comprehensive medication reviews. Effective polypharmacy management in elderly care involves personalized adjustments and interdisciplinary coordination to optimize therapeutic benefits while minimizing potential harms.
Medications Frequently Involved in Polypharmacy
Elderly patients often experience polypharmacy involving medications such as antihypertensives, antidiabetics, and anticoagulants, which are commonly prescribed to manage chronic conditions like hypertension, diabetes, and atrial fibrillation. Statins and proton pump inhibitors are frequently added, increasing the risk of drug interactions and adverse effects. Careful medication review and deprescribing are essential to optimize therapy and reduce polypharmacy-related complications in older adults.
Adverse Effects Linked to Multiple Medications
Elderly patients often experience adverse effects from polypharmacy, such as increased risk of confusion, falls, and gastrointestinal bleeding due to the combined impact of medications like benzodiazepines, anticoagulants, and nonsteroidal anti-inflammatory drugs (NSAIDs). Drug-drug interactions in polypharmacy can exacerbate cognitive decline and lead to hospitalizations, highlighting the need for careful medication review in geriatric care. Monitoring and deprescribing unnecessary drugs reduces adverse outcomes and improves overall health in elderly populations.
Strategies to Prevent Polypharmacy in Seniors
Implementing comprehensive medication reviews involving pharmacists and primary care providers reduces the risk of adverse drug interactions in elderly patients. Utilizing electronic health records to track prescriptions and deprescribing unnecessary medications helps optimize treatment regimens. Educating seniors and caregivers on medication management enhances adherence and prevents polypharmacy-related complications.
Role of Healthcare Providers in Managing Polypharmacy
Healthcare providers play a critical role in managing polypharmacy among elderly patients by conducting thorough medication reviews to identify potentially inappropriate prescriptions and reduce adverse drug interactions. Clinical pharmacists collaborate with physicians to optimize drug regimens, ensuring therapeutic effectiveness while minimizing risks associated with multiple medications. Implementing comprehensive medication management programs and patient education enhances adherence and supports safer pharmacotherapy in geriatric care.
Medication Review Protocols for the Elderly
Polypharmacy in elderly patients, often defined as the concurrent use of five or more medications, increases risks of adverse drug reactions and hospitalizations. Medication Review Protocols for the Elderly, such as the STOPP/START criteria and Beers Criteria, provide structured frameworks to identify potentially inappropriate prescriptions and optimize therapeutic outcomes. Implementing regular, comprehensive medication reviews in geriatric care reduces polypharmacy-related complications and enhances medication safety.
Patient Education and Safe Medication Practices
Elderly patients often face polypharmacy, managing multiple medications for chronic conditions like hypertension, diabetes, and arthritis. Patient education emphasizes understanding each drug's purpose, dosage, and possible interactions to prevent adverse effects. Promoting safe medication practices includes regular medication reviews, using pill organizers, and clear communication with healthcare providers.
example of polypharmacy in elderly Infographic
 samplerz.com
samplerz.com