Marasmus is a severe form of malnutrition primarily caused by a deficiency of calories and protein. It commonly affects infants and young children in regions with insufficient food supply and poor sanitation. Symptoms of marasmus include extreme weight loss, muscle wasting, and a significant reduction in fat stores. The condition is often diagnosed by observing physical signs such as thin, fragile skin and a prominent rib cage due to the loss of subcutaneous fat. Laboratory tests typically reveal low serum albumin and electrolyte imbalances. Treatment involves gradual nutritional rehabilitation with balanced diets rich in energy and protein, along with addressing any underlying infections or health issues.
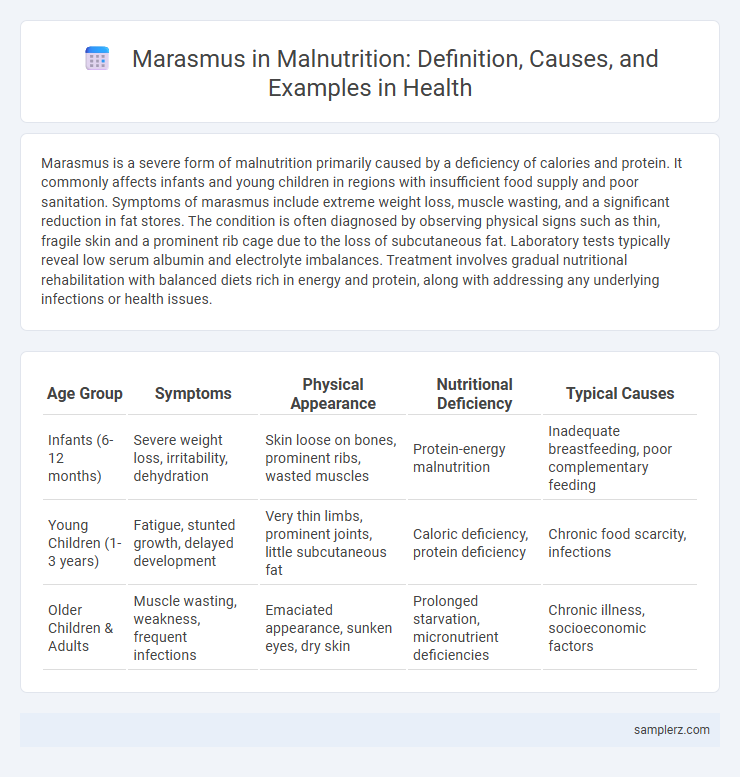
Table of Comparison
| Age Group | Symptoms | Physical Appearance | Nutritional Deficiency | Typical Causes |
|---|---|---|---|---|
| Infants (6-12 months) | Severe weight loss, irritability, dehydration | Skin loose on bones, prominent ribs, wasted muscles | Protein-energy malnutrition | Inadequate breastfeeding, poor complementary feeding |
| Young Children (1-3 years) | Fatigue, stunted growth, delayed development | Very thin limbs, prominent joints, little subcutaneous fat | Caloric deficiency, protein deficiency | Chronic food scarcity, infections |
| Older Children & Adults | Muscle wasting, weakness, frequent infections | Emaciated appearance, sunken eyes, dry skin | Prolonged starvation, micronutrient deficiencies | Chronic illness, socioeconomic factors |
Understanding Marasmus in the Context of Malnutrition
Marasmus is a severe form of protein-energy malnutrition characterized by extreme wasting and muscle loss due to inadequate caloric intake, commonly affecting infants and young children in resource-limited settings. The condition results from prolonged deficiency of all macronutrients, leading to impaired growth, weakened immunity, and increased susceptibility to infections. Understanding marasmus is critical for implementing effective nutritional rehabilitation and preventive strategies to reduce childhood morbidity and mortality globally.
Key Signs and Symptoms of Marasmus
Marasmus is characterized by severe wasting of muscle and fat tissues, leading to an emaciated appearance with prominent ribs and loose, hanging skin. Key signs include stunted growth, fatigue, irritability, and impaired immune function, increasing vulnerability to infections. Children with marasmus often present with a sparse hair texture and dry, flaky skin due to profound energy deficiency.
Causes and Risk Factors of Marasmus in Children
Marasmus in children is primarily caused by severe calorie and protein deficiency due to prolonged inadequate food intake, often linked to poverty and food insecurity. Risk factors include chronic infections, such as diarrhea and respiratory illnesses, which increase nutrient loss and energy requirements, as well as poor breastfeeding practices and lack of access to nutritious complementary foods. Environmental factors like poor sanitation and limited healthcare access further exacerbate the vulnerability to marasmus in young children.
Diagnosing Marasmus: Clinical Indicators
Diagnosing marasmus involves identifying severe wasting, characterized by a marked loss of muscle mass and subcutaneous fat, evident in a child with a drastically low weight-for-height ratio below -3 SD of the WHO growth standards. Clinical indicators include visible ribs and bones, prominent skin folds, and extreme lethargy or irritability due to energy deficiency. Accurate diagnosis also considers a history of inadequate caloric intake and absence of edema, distinguishing marasmus from kwashiorkor in malnutrition assessments.
Marasmus vs. Kwashiorkor: Key Differences
Marasmus is characterized by severe energy deficiency resulting in extreme wasting and muscle loss, while Kwashiorkor primarily stems from protein deficiency leading to edema and fatty liver. Unlike Kwashiorkor, marasmus presents with significant weight loss and depletion of fat stores without fluid retention. Understanding these distinctions is crucial for accurate diagnosis and treatment of malnutrition in pediatric patients.
Case Study: Real-Life Example of Marasmus
A case study of marasmus illustrates severe energy deficiency in a 2-year-old child presenting with extreme muscle wasting, stunted growth, and lethargy due to prolonged inadequate caloric intake. Laboratory findings revealed hypoalbuminemia and low serum electrolytes, confirming malnutrition-related metabolic imbalances. Nutritional rehabilitation focused on gradual refeeding and micronutrient supplementation, resulting in significant clinical improvement over several months.
Consequences of Untreated Marasmus
Untreated marasmus leads to severe wasting of muscle and fat tissues, resulting in extreme weakness and susceptibility to infections. Prolonged energy deficiency causes organ damage, impaired immune response, and delayed cognitive development in children. Without timely intervention, marasmus can progress to multi-organ failure and increased mortality risk.
Effective Treatment and Recovery Strategies
Effective treatment of marasmus involves immediate nutritional rehabilitation through carefully monitored refeeding protocols, emphasizing high-calorie, nutrient-dense foods to restore body weight and muscle mass. Supplementation with essential vitamins and minerals, particularly zinc, vitamin A, and iron, supports immune function and tissue repair during recovery. Ongoing medical supervision ensures management of complications and gradual normalization of metabolic processes for sustainable health restoration.
Preventive Measures Against Marasmus
Preventive measures against marasmus in malnutrition prioritize early breastfeeding initiation, exclusive breastfeeding for the first six months, and timely introduction of nutrient-rich complementary foods. Ensuring food security by providing balanced diets with adequate calories, proteins, and micronutrients such as vitamin A, zinc, and iron reduces the risk of severe energy deficiency. Community health programs promoting nutritional education, regular growth monitoring, and sanitation improvements directly contribute to lowering the incidence of marasmus in vulnerable populations.
Community Initiatives Addressing Marasmus and Malnutrition
Community initiatives tackling marasmus and malnutrition include nutrition education programs, supplementary feeding schemes, and improved access to clean water and sanitation. Health workers conduct regular screenings in vulnerable populations to identify early signs of severe acute malnutrition, enabling timely intervention with therapeutic foods. Partnerships between local governments and NGOs enhance distribution of micronutrient supplements and promote breastfeeding, significantly reducing rates of marasmus in affected regions.
example of marasmus in malnutrition Infographic
 samplerz.com
samplerz.com