Mucositis is a common complication in patients undergoing hematopoietic stem cell transplantation (HSCT). It manifests as painful inflammation and ulceration of the mucous membranes lining the digestive tract, particularly the oral cavity. Data indicate that up to 75% of transplant recipients develop mucositis, which can increase the risk of infection and prolong hospital stays. This condition results from the cytotoxic effects of high-dose chemotherapy or radiation therapy used before transplantation. The severity of mucositis is often graded on a scale from 1 to 4, reflecting the extent of tissue damage and symptom intensity. Effective management includes pain control, oral hygiene protocols, and the use of protective agents like palifermin to reduce mucosal injury.
Table of Comparison
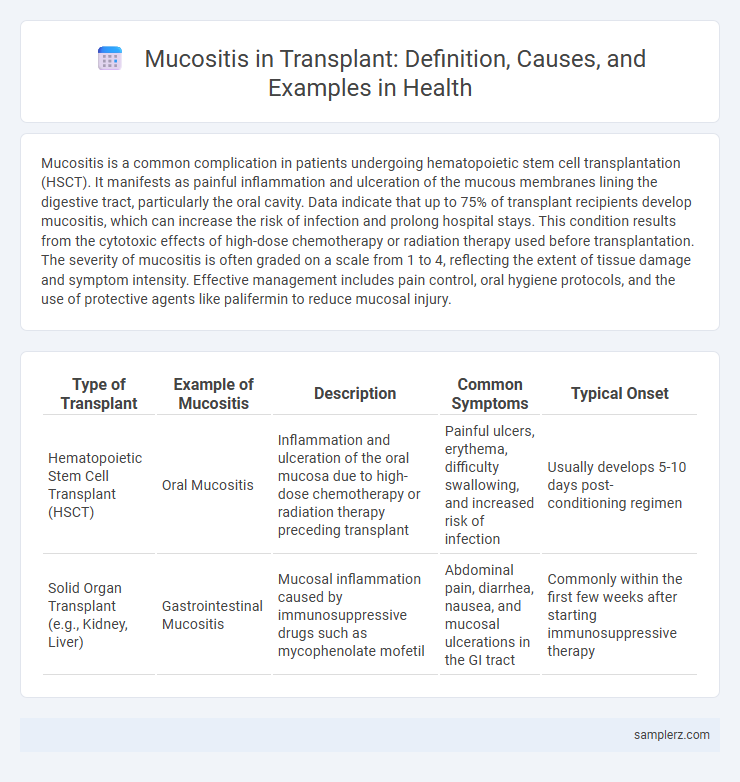
| Type of Transplant | Example of Mucositis | Description | Common Symptoms | Typical Onset |
|---|---|---|---|---|
| Hematopoietic Stem Cell Transplant (HSCT) | Oral Mucositis | Inflammation and ulceration of the oral mucosa due to high-dose chemotherapy or radiation therapy preceding transplant | Painful ulcers, erythema, difficulty swallowing, and increased risk of infection | Usually develops 5-10 days post-conditioning regimen |
| Solid Organ Transplant (e.g., Kidney, Liver) | Gastrointestinal Mucositis | Mucosal inflammation caused by immunosuppressive drugs such as mycophenolate mofetil | Abdominal pain, diarrhea, nausea, and mucosal ulcerations in the GI tract | Commonly within the first few weeks after starting immunosuppressive therapy |
Understanding Mucositis in Transplant Patients
Mucositis in transplant patients typically manifests as painful inflammation and ulceration of the mucous membranes, often triggered by high-dose chemotherapy or radiation therapy used during conditioning regimens. This condition significantly increases the risk of infection due to the compromised mucosal barrier and can prolong hospital stays, impacting overall transplant outcomes. Effective management strategies include maintaining oral hygiene, pain control with topical analgesics, and the use of growth factors like palifermin to promote mucosal healing.
Common Causes of Mucositis During Transplantation
Mucositis during transplantation commonly results from high-dose chemotherapy and total body irradiation, which damage the rapidly dividing epithelial cells of the mucous membranes. Immunosuppressive drugs used to prevent graft rejection can also contribute to the development of mucositis by delaying mucosal healing. Infection by opportunistic pathogens such as Candida species frequently exacerbates the condition in transplant patients.
Clinical Presentation: Signs and Symptoms of Mucositis
Mucositis in transplant patients typically presents with erythema and painful ulcerations along the oral mucosa, leading to difficulty in swallowing and speaking. Symptoms often include severe oral pain, dry mouth, and a burning sensation, which can compromise nutritional intake and increase the risk of secondary infections. Clinically, mucosal swelling and bleeding may be observed, significantly impacting patient comfort and recovery post-transplant.
Oral Mucositis: Prevalence in Stem Cell Transplant
Oral mucositis is a common and severe complication affecting approximately 75% to 99% of patients undergoing hematopoietic stem cell transplantation (HSCT). It results from the cytotoxic effects of high-dose chemotherapy and radiation, causing painful ulcerations that impair oral intake and increase infection risk. Effective management strategies include prophylactic oral care protocols and emerging agents like palifermin that promote mucosal healing and reduce mucositis severity.
Gastrointestinal Mucositis: Key Manifestations Post-Transplant
Gastrointestinal mucositis frequently occurs after hematopoietic stem cell transplantation, characterized by severe oral ulcers, abdominal pain, and diarrhea due to epithelial damage in the digestive tract. This condition results from cytotoxic effects of conditioning regimens such as chemotherapy and total body irradiation, leading to inflammation and compromised mucosal integrity. Effective management includes pain control, nutritional support, and prophylactic measures to prevent secondary infections and improve patient outcomes.
Case Study: Severe Mucositis Following Bone Marrow Transplant
Severe mucositis commonly occurs in patients undergoing bone marrow transplants due to high-dose chemotherapy and radiation therapy that damage the mucosal lining of the mouth and gastrointestinal tract. A case study detailed a patient experiencing extensive oral ulcerations, intense pain, and impaired nutrition requiring opioid analgesics and parenteral nutrition support. Management involved multidisciplinary care, including antimicrobial prophylaxis and specialized wound care to promote mucosal healing and prevent secondary infections.
Risk Factors for Mucositis in Hematopoietic Stem Cell Recipients
Mucositis in hematopoietic stem cell transplant recipients is commonly triggered by high-dose chemotherapy and total body irradiation used in conditioning regimens. Risk factors include older age, poor oral hygiene, and pre-existing oral infections, which exacerbate mucosal barrier injury. Genetic predispositions, such as variations in enzymes like methylenetetrahydrofolate reductase (MTHFR), also influence individual susceptibility to mucositis.
Diagnostic Approaches: Identifying Mucositis in Transplant Recipients
Mucositis in transplant recipients is commonly diagnosed through clinical examination, highlighting erythema, ulcerations, and pain in the oral mucosa. Diagnostic approaches often include direct visualization, alongside biopsy and histopathological analysis to differentiate from infections or graft-versus-host disease. Advanced techniques such as fluorescence imaging and biomarkers in saliva may enhance early detection and severity assessment of mucositis in post-transplant care.
Management Strategies for Mucositis During and After Transplant
Management strategies for mucositis during and after transplant prioritize pain control using topical analgesics and systemic opioids to improve patient comfort. Maintaining rigorous oral hygiene with saline or baking soda rinses helps reduce infection risk and promote healing. Nutritional support through enteral feeding and hydration is crucial to prevent weight loss and support mucosal recovery in transplant patients.
Preventive Measures to Reduce Mucositis Risk in Transplant Patients
Effective preventive measures to reduce mucositis risk in transplant patients include maintaining rigorous oral hygiene through regular brushing and antimicrobial mouth rinses, which help minimize oral microbial load and tissue irritation. Use of cryotherapy, such as ice chips during chemotherapy infusion, has demonstrated significant reduction in mucosal injury by constricting blood vessels and limiting cytotoxic exposure. Administering growth factors like palifermin promotes mucosal cell regeneration, further decreasing the incidence and severity of mucositis post-transplant.
example of mucositis in transplant Infographic
 samplerz.com
samplerz.com