Polypharmacy in geriatric patients often involves the simultaneous use of multiple medications to manage chronic conditions such as hypertension, diabetes, and arthritis. For example, an elderly patient might be prescribed antihypertensives, antidiabetics, and nonsteroidal anti-inflammatory drugs (NSAIDs) concurrently. This practice increases the risk of adverse drug reactions and drug-drug interactions due to the complexity of managing diverse pharmacological treatments. Data from healthcare studies show that over 40% of individuals aged 65 and older take five or more medications daily, illustrating the prevalence of polypharmacy in this demographic. Common entities involved include general practitioners, pharmacists, and geriatricians who monitor and adjust medication regimens to optimize therapeutic outcomes. Effective management of polypharmacy requires comprehensive medication reviews and patient education to minimize risks and enhance the quality of life for elderly patients.
Table of Comparison
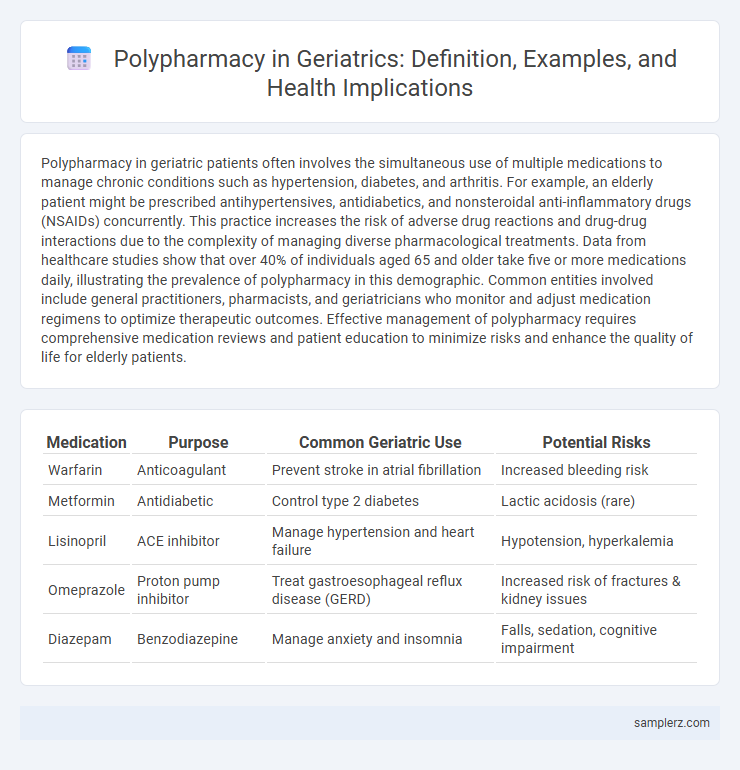
| Medication | Purpose | Common Geriatric Use | Potential Risks |
|---|---|---|---|
| Warfarin | Anticoagulant | Prevent stroke in atrial fibrillation | Increased bleeding risk |
| Metformin | Antidiabetic | Control type 2 diabetes | Lactic acidosis (rare) |
| Lisinopril | ACE inhibitor | Manage hypertension and heart failure | Hypotension, hyperkalemia |
| Omeprazole | Proton pump inhibitor | Treat gastroesophageal reflux disease (GERD) | Increased risk of fractures & kidney issues |
| Diazepam | Benzodiazepine | Manage anxiety and insomnia | Falls, sedation, cognitive impairment |
Common Drug Combinations in Elderly Polypharmacy
Common drug combinations in elderly polypharmacy often include antihypertensives such as ACE inhibitors paired with diuretics to manage hypertension, alongside statins for cholesterol control. Elderly patients frequently receive combinations of anticoagulants like warfarin with antiplatelet agents, increasing the risk of bleeding complications. Additionally, concurrent use of benzodiazepines with opioids is prevalent for managing anxiety and pain but requires careful monitoring to avoid adverse effects.
Frequently Prescribed Medications in Geriatric Patients
Older adults often experience polypharmacy due to multiple chronic conditions requiring treatment with medications such as antihypertensives, statins, anticoagulants, and antidiabetics. Commonly prescribed drugs include beta-blockers for hypertension, metformin for diabetes management, and low-dose aspirin for cardiovascular protection. Monitoring for drug interactions and adverse effects is essential to optimize therapeutic outcomes and ensure patient safety in geriatric care.
Case Studies: Polypharmacy Scenarios in Older Adults
A common example of polypharmacy in geriatric patients involves an 82-year-old with hypertension, type 2 diabetes, and osteoarthritis prescribed seven medications, including beta-blockers, metformin, and NSAIDs. Case studies reveal risks such as adverse drug interactions and increased hospitalizations due to inappropriate drug combinations. Clinical management emphasizes regular medication reviews and deprescribing protocols to reduce polypharmacy-related complications in older adults.
High-Risk Medication Interactions in Geriatrics
Polypharmacy in geriatric patients often involves the concurrent use of medications such as anticoagulants, antiplatelets, and nonsteroidal anti-inflammatory drugs (NSAIDs), which can lead to high-risk drug interactions causing bleeding complications or renal impairment. Common high-risk medication interactions include combining warfarin with aspirin or NSAIDs, increasing the risk of gastrointestinal bleeding. Managing these interactions requires careful medication reconciliation and monitoring to prevent adverse drug events in elderly patients.
Chronic Disease Polypharmacy Examples in Seniors
Chronic disease polypharmacy in seniors often includes the simultaneous use of antihypertensives, statins, and antidiabetic medications to manage hypertension, high cholesterol, and diabetes mellitus. Common regimens also involve anticoagulants like warfarin or direct oral anticoagulants alongside medications for chronic obstructive pulmonary disease (COPD) and osteoarthritis pain management. This complex medication use increases the risk of adverse drug interactions and requires careful monitoring in geriatric patients.
Polypharmacy in Dementia Care: Drug Examples
In geriatric dementia care, polypharmacy commonly involves medications such as donepezil, memantine, antipsychotics like risperidone, and benzodiazepines prescribed to manage cognitive symptoms, behavioral disturbances, and sleep issues. The concurrent use of cholinesterase inhibitors with anticholinergic drugs increases the risk of adverse drug interactions and cognitive decline. Careful medication review and deprescribing strategies are essential to minimize polypharmacy risks and optimize therapeutic outcomes in elderly dementia patients.
Cardiometabolic Polypharmacy Profiles in Elderly
Cardiometabolic polypharmacy in elderly patients typically involves the concurrent use of antihypertensives, statins, and oral hypoglycemic agents to manage complex conditions like hypertension, hyperlipidemia, and type 2 diabetes mellitus. This polypharmacy profile increases the risk of adverse drug interactions, leading to potential complications such as hypotension, hypoglycemia, and impaired renal function. Effective management requires regular medication reviews and personalized therapeutic strategies to optimize clinical outcomes and minimize side effects in geriatric populations.
Adverse Reactions from Polypharmacy: Real-life Cases
Elderly patients often experience adverse reactions from polypharmacy, such as increased risk of falls, confusion, and gastrointestinal bleeding. A common example includes the combined use of anticoagulants like warfarin with nonsteroidal anti-inflammatory drugs (NSAIDs), which significantly raises the likelihood of hemorrhagic complications. Real-life cases reveal that careful medication review and monitoring are critical to preventing these potentially life-threatening side effects in geriatric populations.
Preventable Polypharmacy in the Aging Population
Preventable polypharmacy in the aging population often involves the unnecessary use of multiple medications such as benzodiazepines, proton pump inhibitors, and anticholinergics, which increase the risk of adverse drug reactions and hospitalizations. Studies show that up to 30% of geriatric patients experience medication duplication or inappropriate prescriptions, highlighting the need for regular medication reviews and deprescribing protocols. Implementing clinical guidelines and pharmacist-led interventions significantly reduces preventable polypharmacy and improves health outcomes in older adults.
Polypharmacy and Functional Decline: Illustrative Cases
Polypharmacy in geriatric patients often involves managing multiple chronic conditions such as hypertension, diabetes, and arthritis, with an average of five or more medications prescribed simultaneously. This complex medication regimen increases the risk of adverse drug reactions, leading to functional decline manifested as reduced mobility, cognitive impairment, or increased fall risk. Case studies reveal that careful medication review and deprescribing strategies can help mitigate these negative outcomes and improve overall quality of life for elderly patients.
example of polypharmacy in geriatric Infographic
 samplerz.com
samplerz.com