Orthopnea is a common symptom in cardiology characterized by difficulty breathing when lying flat. Patients with congestive heart failure often experience orthopnea due to the redistribution of body fluids, which increases pulmonary congestion. Data shows that the severity of orthopnea correlates with worsening left ventricular function and elevated pulmonary capillary wedge pressure. In clinical practice, orthopnea is assessed by noting the number of pillows a patient uses to sleep comfortably, often referred to as the "pillows test." This symptom provides valuable diagnostic information for physicians managing chronic heart conditions. Research confirms that the presence of orthopnea can predict adverse outcomes and guide tailored treatment strategies for heart failure patients.
Table of Comparison
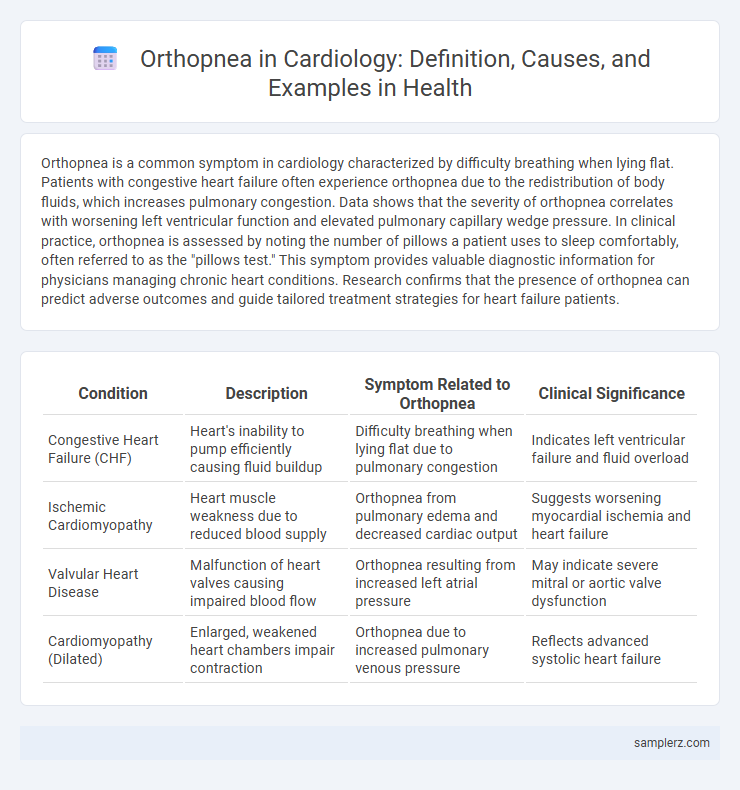
| Condition | Description | Symptom Related to Orthopnea | Clinical Significance |
|---|---|---|---|
| Congestive Heart Failure (CHF) | Heart's inability to pump efficiently causing fluid buildup | Difficulty breathing when lying flat due to pulmonary congestion | Indicates left ventricular failure and fluid overload |
| Ischemic Cardiomyopathy | Heart muscle weakness due to reduced blood supply | Orthopnea from pulmonary edema and decreased cardiac output | Suggests worsening myocardial ischemia and heart failure |
| Valvular Heart Disease | Malfunction of heart valves causing impaired blood flow | Orthopnea resulting from increased left atrial pressure | May indicate severe mitral or aortic valve dysfunction |
| Cardiomyopathy (Dilated) | Enlarged, weakened heart chambers impair contraction | Orthopnea due to increased pulmonary venous pressure | Reflects advanced systolic heart failure |
Definition and Overview of Orthopnea in Cardiology
Orthopnea in cardiology refers to difficulty breathing when lying flat, commonly caused by left ventricular heart failure. This symptom occurs due to pulmonary congestion from increased venous return in the supine position, leading to fluid accumulation in the lungs. Patients often require multiple pillows or elevated sleeping positions to alleviate respiratory distress effectively.
Common Symptoms Associated with Orthopnea
Orthopnea in cardiology commonly presents with symptoms such as shortness of breath when lying flat, which typically improves upon sitting or standing. Patients often report nocturnal dyspnea and may experience fatigue due to disrupted sleep. These symptoms are frequently linked to congestive heart failure and impaired left ventricular function.
Pathophysiology: How Orthopnea Develops in Heart Patients
Orthopnea in cardiology arises due to left ventricular failure, where the heart's inability to pump efficiently leads to increased pulmonary venous pressure and fluid accumulation in the lungs. This gravitational shift during lying down causes pulmonary congestion, triggering shortness of breath. The resulting impaired gas exchange and lung stiffness intensify respiratory distress when patients adopt a supine position.
Key Causes of Orthopnea in Cardiac Conditions
Orthopnea commonly occurs in patients with left ventricular failure, where the heart's reduced pumping capacity leads to fluid accumulation in the lungs when lying flat. Mitral valve disease, particularly mitral stenosis or regurgitation, contributes to increased pulmonary venous pressure, resulting in orthopnea. Chronic heart failure and ischemic cardiomyopathy are also primary cardiac conditions causing this symptom due to impaired cardiac output and pulmonary congestion.
Clinical Examples of Orthopnea in Heart Failure
Orthopnea is commonly observed in patients with congestive heart failure, where left ventricular dysfunction leads to pulmonary congestion when lying flat. Clinical examples include dyspnea worsening upon supine position, requiring multiple pillows for sleep, reflecting elevated left atrial pressure. This symptom is indicative of fluid redistribution and increased pulmonary capillary pressure, characteristic of heart failure progression.
Patient Case Study: Presenting with Orthopnea
A 65-year-old male patient with a history of congestive heart failure presented with orthopnea, experiencing difficulty breathing while lying flat and requiring multiple pillows to sleep comfortably. Physical examination revealed elevated jugular venous pressure and bilateral basal crackles, indicating pulmonary congestion secondary to left ventricular dysfunction. Echocardiography confirmed reduced ejection fraction, correlating with clinical symptoms of orthopnea related to fluid overload and impaired cardiac output.
Diagnostic Approaches for Detecting Orthopnea
Orthopnea, characterized by difficulty breathing while lying flat, is a common symptom in patients with congestive heart failure, necessitating precise diagnostic approaches. Diagnostic strategies include detailed patient history, physical examination focusing on pulmonary crackles and jugular venous distension, and confirmatory tests such as chest X-ray to assess pulmonary edema and echocardiography to evaluate ventricular function. Additionally, measuring brain natriuretic peptide (BNP) levels aids in distinguishing cardiac causes of orthopnea from pulmonary conditions.
Management Strategies for Cardiac-Related Orthopnea
Orthopnea in cardiology typically manifests as difficulty breathing when lying flat, often indicating left ventricular heart failure. Management strategies focus on optimizing heart failure treatment through diuretics to reduce pulmonary congestion, angiotensin-converting enzyme (ACE) inhibitors to improve cardiac function, and beta-blockers to decrease myocardial oxygen demand. Positioning techniques, such as elevating the head of the bed, complement pharmacological interventions by alleviating respiratory distress during recumbency.
Prognostic Significance of Orthopnea in Cardiology
Orthopnea, characterized by difficulty breathing when lying flat, is a critical symptom in cardiology often associated with heart failure and left ventricular dysfunction. Its presence indicates elevated left atrial pressure and pulmonary congestion, serving as a prognostic marker for worsened cardiac outcomes and increased mortality risk. Monitoring orthopnea severity helps clinicians stratify patient risk and tailor heart failure management strategies effectively.
Preventive Measures to Reduce Orthopnea Episodes in Patients
Orthopnea in cardiology often manifests as difficulty breathing when lying flat, commonly seen in patients with congestive heart failure. Preventive measures to reduce orthopnea episodes include optimizing fluid balance through diuretics, maintaining a low-sodium diet to prevent fluid retention, and using elevated head-of-bed positioning during sleep. Regular monitoring of cardiac function and adherence to prescribed medications also play a crucial role in minimizing the frequency and severity of orthopnea symptoms.
example of orthopnea in cardiology Infographic
 samplerz.com
samplerz.com