Schizophrenia and substance use disorder often co-occur as a common comorbidity in psychiatric disorders. Research data indicates that approximately 50% of individuals with schizophrenia experience substance abuse issues, exacerbating symptoms and complicating treatment. This comorbidity significantly influences disease progression and necessitates integrated therapeutic approaches for better health outcomes. Anxiety disorders frequently coexist with major depressive disorder, forming another prevalent comorbid psychiatric condition. Clinical studies report that about 60% of patients diagnosed with depression also exhibit symptoms of anxiety. Understanding this overlap is critical for precise diagnosis and personalized treatment plans targeting the interconnected nature of these mental health disorders.
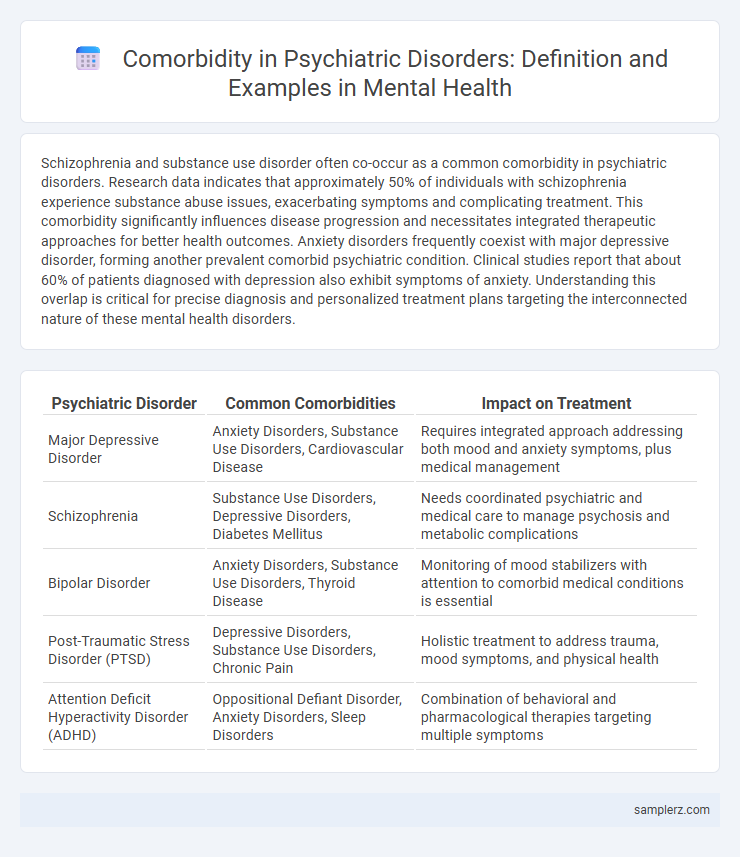
Table of Comparison
| Psychiatric Disorder | Common Comorbidities | Impact on Treatment |
|---|---|---|
| Major Depressive Disorder | Anxiety Disorders, Substance Use Disorders, Cardiovascular Disease | Requires integrated approach addressing both mood and anxiety symptoms, plus medical management |
| Schizophrenia | Substance Use Disorders, Depressive Disorders, Diabetes Mellitus | Needs coordinated psychiatric and medical care to manage psychosis and metabolic complications |
| Bipolar Disorder | Anxiety Disorders, Substance Use Disorders, Thyroid Disease | Monitoring of mood stabilizers with attention to comorbid medical conditions is essential |
| Post-Traumatic Stress Disorder (PTSD) | Depressive Disorders, Substance Use Disorders, Chronic Pain | Holistic treatment to address trauma, mood symptoms, and physical health |
| Attention Deficit Hyperactivity Disorder (ADHD) | Oppositional Defiant Disorder, Anxiety Disorders, Sleep Disorders | Combination of behavioral and pharmacological therapies targeting multiple symptoms |
Understanding Comorbidity in Psychiatric Disorders
Comorbidity in psychiatric disorders often includes the simultaneous occurrence of major depressive disorder and generalized anxiety disorder, which frequently complicates diagnosis and treatment strategies. Studies indicate that nearly 60% of individuals diagnosed with depression also exhibit symptoms of anxiety, highlighting the need for integrated therapeutic approaches. Recognizing such comorbid conditions improves personalized care plans and enhances patient outcomes in mental health settings.
Common Psychiatric Comorbidity Examples
Depression frequently co-occurs with anxiety disorders, creating a complex clinical profile that complicates diagnosis and treatment. Substance use disorders commonly appear alongside bipolar disorder, amplifying symptom severity and increasing the risk of relapse. Post-traumatic stress disorder (PTSD) often presents with comorbid major depressive disorder, leading to heightened impairment and a greater need for integrated therapeutic approaches.
Depression and Anxiety: A Frequent Comorbid Pair
Depression and anxiety often coexist, with studies showing that up to 60% of patients diagnosed with major depressive disorder also experience generalized anxiety disorder. This comorbidity exacerbates symptom severity, complicates treatment strategies, and increases the risk of chronic illness. Effective management requires integrated therapeutic approaches targeting both mood and anxiety symptoms to improve patient outcomes.
Substance Use Disorders and Psychiatric Comorbidity
Substance Use Disorders frequently co-occur with psychiatric disorders such as major depression, anxiety disorders, and schizophrenia, complicating diagnosis and treatment. Epidemiological studies indicate that approximately 50% of individuals with psychiatric disorders also experience substance abuse, leading to increased hospitalization and poorer treatment outcomes. Integrated care models targeting both substance use and psychiatric symptoms simultaneously demonstrate improved recovery rates and reduced relapse.
Bipolar Disorder with Co-occurring Conditions
Bipolar disorder commonly co-occurs with anxiety disorders, substance use disorders, and attention-deficit/hyperactivity disorder (ADHD), complicating diagnosis and treatment. The presence of comorbid anxiety increases the risk of mood instability and suicide attempts in individuals with bipolar disorder. Integrated therapeutic approaches targeting both mood symptoms and co-occurring conditions improve overall outcomes and reduce hospitalization rates.
Schizophrenia and Comorbid Medical Disorders
Schizophrenia frequently presents with comorbid medical disorders such as cardiovascular disease, diabetes mellitus, and respiratory conditions, significantly impacting morbidity and mortality rates. The prevalence of metabolic syndrome in schizophrenic patients is notably high due to antipsychotic medication side effects and lifestyle factors, exacerbating cardiovascular risks. Effective management requires integrated care approaches addressing both psychiatric symptoms and concurrent medical conditions to improve overall patient outcomes.
ADHD and Its Psychiatric Comorbidities
Attention Deficit Hyperactivity Disorder (ADHD) commonly co-occurs with psychiatric comorbidities such as anxiety disorders, depression, and oppositional defiant disorder (ODD). Studies indicate that up to 50% of individuals with ADHD experience at least one comorbid psychiatric condition, complicating diagnosis and treatment. Understanding the interplay between ADHD and its comorbidities is crucial for developing comprehensive mental health interventions.
Personality Disorders and Their Comorbidity Patterns
Personality disorders frequently co-occur with mood disorders, anxiety disorders, and substance use disorders, complicating diagnosis and treatment. Borderline personality disorder often presents with comorbid major depressive disorder and post-traumatic stress disorder, while antisocial personality disorder is strongly linked to substance abuse disorders. Understanding these comorbidity patterns enhances clinical outcomes by informing integrated treatment approaches tailored to the complex interplay of psychiatric conditions.
Challenges in Diagnosing Psychiatric Comorbidities
Diagnostic challenges in psychiatric comorbidities arise from overlapping symptoms between disorders such as major depressive disorder and anxiety disorders, which complicate clinical assessments. The presence of co-occurring conditions like bipolar disorder and substance use disorder often leads to misdiagnosis or delayed treatment, impacting patient outcomes. Accurate identification requires comprehensive evaluation strategies, incorporating structured interviews and standardized rating scales tailored to detect multiple psychiatric diagnoses concurrently.
Managing Comorbidity in Mental Health Treatment
Managing comorbidity in mental health treatment requires an integrated approach addressing both psychiatric disorders such as depression and anxiety and co-occurring conditions like substance use or chronic medical illnesses. Evidence-based interventions combining pharmacotherapy and psychotherapy tailored to individual patient profiles improve treatment outcomes and reduce relapse rates. Collaborative care models involving multidisciplinary teams enhance coordination, monitoring, and comprehensive support for patients with complex comorbidities.
example of comorbidity in psychiatric disorder Infographic
 samplerz.com
samplerz.com