Meningocele is a form of spina bifida characterized by the protrusion of the meninges through a defect in the vertebral column. This condition involves the sac-like cyst filled with cerebrospinal fluid, but the spinal cord remains in its normal position. Meningocele is detected through prenatal imaging techniques such as ultrasound and MRI, which reveal the abnormal spinal opening. The severity of meningocele varies, with symptoms ranging from minor physical disabilities to neurological complications. Surgical intervention is typically required to close the spinal defect and prevent infections like meningitis. Long-term management includes physical therapy and regular neurological assessments to monitor motor function and development.
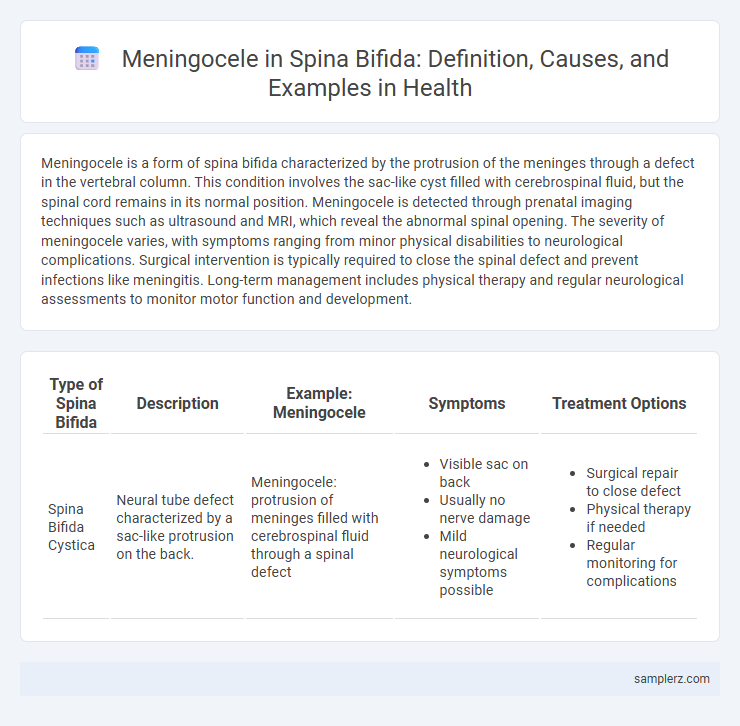
Table of Comparison
| Type of Spina Bifida | Description | Example: Meningocele | Symptoms | Treatment Options |
|---|---|---|---|---|
| Spina Bifida Cystica | Neural tube defect characterized by a sac-like protrusion on the back. | Meningocele: protrusion of meninges filled with cerebrospinal fluid through a spinal defect |
|
|
Understanding Meningocele: A Form of Spina Bifida
Meningocele, a type of spina bifida, occurs when the protective membranes around the spinal cord push through a vertebral opening, forming a sac filled with cerebrospinal fluid. Unlike myelomeningocele, this condition typically does not involve the spinal cord itself, often resulting in milder neurological symptoms. Early diagnosis through prenatal imaging and timely surgical intervention can significantly improve outcomes and reduce complications associated with meningoceles.
Key Characteristics of Meningocele in Spina Bifida
Meningocele in spina bifida is characterized by the protrusion of the meninges through a defect in the vertebral arches, forming a cerebrospinal fluid-filled sac visible on the back. Unlike myelomeningocele, the spinal cord remains normally positioned without neural tissue involvement, resulting in milder neurological symptoms. Common key features include a visible sac covered by skin, potential hydrocephalus, and varying degrees of motor or sensory impairment depending on the lesion's location.
Causes and Risk Factors for Meningocele Development
Meningocele, a form of spina bifida, develops when the neural tube fails to close properly during fetal development, leading to the protrusion of the meninges through an opening in the spine. Key risk factors include maternal folic acid deficiency, genetic predispositions, and environmental exposures such as maternal diabetes and certain medications. Advanced maternal age and obesity also contribute to the increased likelihood of meningocele formation in newborns.
Clinical Presentation: How Meningocele Appears
Meningocele in spina bifida presents as a visible sac protruding through a defect in the vertebral column, typically on the lower back. The sac contains meninges and cerebrospinal fluid but does not include neural tissue, often resulting in mild or no neurological deficits. Clinical signs include a soft, cystic swelling covered by skin, without associated paralysis or sensory loss in most cases.
Diagnostic Approaches for Meningocele in Spina Bifida
Diagnostic approaches for meningocele in spina bifida primarily involve prenatal ultrasound and fetal MRI to identify the characteristic cerebrospinal fluid-filled sac protruding through vertebral defects. Postnatal diagnosis is confirmed through physical examination and imaging techniques such as spinal X-rays, ultrasonography, and MRI to assess the extent of the neural tissue involvement and sac contents. Early and accurate detection through these imaging modalities is crucial for planning surgical intervention and preventing neurological complications.
Treatment Options for Meningocele Cases
Treatment options for meningocele, a form of spina bifida, primarily involve surgical repair to close the spinal defect and prevent infection. Postoperative care includes monitoring for cerebrospinal fluid leaks, managing neurological symptoms, and physical therapy to improve mobility and prevent complications. Early intervention significantly improves outcomes by reducing the risk of further neural damage and promoting normal development.
Real-Life Example: Case Study of Meningocele
A newborn diagnosed with meningocele, a subtype of spina bifida, presented with a sac-like protrusion on the lower spine containing cerebrospinal fluid but no spinal cord involvement. Surgical intervention within the first days of life successfully repaired the defect, preventing infections and minimizing neurological damage. Follow-up assessments indicated normal motor function and cognitive development, highlighting the effectiveness of early diagnosis and treatment in meningocele cases.
Possible Complications in Meningocele
Meningocele in spina bifida can lead to complications such as cerebrospinal fluid leakage, which increases the risk of meningitis and other infections. Neurological impairments including motor weakness or sensory deficits may occur if nerve tissue is affected by the condition. Early surgical intervention reduces the likelihood of severe complications and improves long-term outcomes for patients with meningocele.
Prognosis and Long-Term Outlook for Meningocele Patients
Meningocele, a form of spina bifida characterized by the protrusion of meninges through a spinal defect, generally has a favorable prognosis when treated promptly. Most patients experience minimal neurological impairment and can lead normal lives with appropriate surgical repair and ongoing rehabilitation. Long-term outlook includes regular monitoring for potential complications such as tethered cord syndrome and hydrocephalus to ensure optimal neurological function.
Prevention Strategies for Spina Bifida and Meningocele
Folic acid supplementation before conception and during early pregnancy reduces the risk of spina bifida and meningocele by promoting proper neural tube closure. Prenatal screening through ultrasound and maternal serum alpha-fetoprotein testing facilitates early detection and informed management of neural tube defects. Public health initiatives emphasizing nutrition education and access to prenatal care are critical components in preventing meningocele associated with spina bifida.
example of meningocele in spina bifida Infographic
 samplerz.com
samplerz.com