Hyperalgesia is a condition characterized by an increased sensitivity to pain, often resulting from nerve damage or chronic inflammation. A common example of hyperalgesia occurs in patients with diabetic neuropathy, where minor stimuli such as a light touch can cause intense pain sensations. This heightened pain response is due to changes in both peripheral and central nervous system pathways that amplify pain signals. In clinical settings, hyperalgesia is frequently observed following opioid use, known as opioid-induced hyperalgesia, where patients experience worsening pain despite escalating opioid doses. Experimental models demonstrate that hyperalgesia can be measured using quantitative sensory testing, which assesses pain thresholds and responses to thermal or mechanical stimuli. Understanding hyperalgesia's underlying mechanisms aids in developing targeted treatments to mitigate excessive pain perception.
Table of Comparison
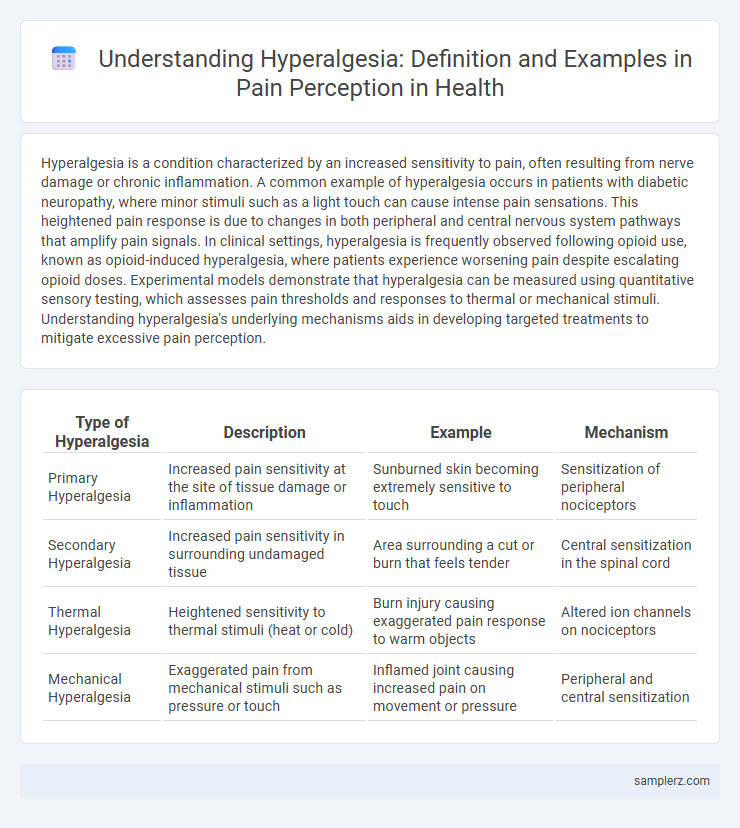
| Type of Hyperalgesia | Description | Example | Mechanism |
|---|---|---|---|
| Primary Hyperalgesia | Increased pain sensitivity at the site of tissue damage or inflammation | Sunburned skin becoming extremely sensitive to touch | Sensitization of peripheral nociceptors |
| Secondary Hyperalgesia | Increased pain sensitivity in surrounding undamaged tissue | Area surrounding a cut or burn that feels tender | Central sensitization in the spinal cord |
| Thermal Hyperalgesia | Heightened sensitivity to thermal stimuli (heat or cold) | Burn injury causing exaggerated pain response to warm objects | Altered ion channels on nociceptors |
| Mechanical Hyperalgesia | Exaggerated pain from mechanical stimuli such as pressure or touch | Inflamed joint causing increased pain on movement or pressure | Peripheral and central sensitization |
Understanding Hyperalgesia: Definition and Mechanisms
Hyperalgesia is characterized by an increased sensitivity to pain, often resulting from nerve injury or inflammation. This condition involves the sensitization of peripheral nociceptors and central nervous system pathways, leading to amplified pain signals. Common examples include enhanced pain response to normally painful stimuli in conditions such as neuropathic pain and chronic inflammation.
Acute Injury Hyperalgesia: Pain Beyond the Initial Wound
Acute Injury Hyperalgesia occurs when pain sensitivity increases significantly around the site of an injury, extending beyond the immediate wound area. This heightened pain response involves peripheral sensitization, where nociceptors become more reactive, and central sensitization, amplifying pain signals in the spinal cord. Common examples include increased pain intensity after a burn or surgical incision, where even light touch or mild pressure induces exaggerated discomfort.
Post-Surgical Hyperalgesia: Enhanced Pain After Operations
Post-surgical hyperalgesia manifests as increased sensitivity to pain following surgical procedures, often caused by nerve injury or inflammation. This condition results from central sensitization mechanisms, where the nervous system amplifies pain signals, leading to exaggerated pain responses at the surgical site. Effective management includes multimodal analgesia targeting both peripheral and central pain pathways to reduce hyperalgesic effects and improve patient recovery outcomes.
Opioid-Induced Hyperalgesia: Paradoxical Pain from Medication
Opioid-Induced Hyperalgesia (OIH) occurs when long-term opioid use paradoxically heightens a patient's sensitivity to pain, resulting in increased discomfort despite escalating doses. This condition challenges pain management as opioids, meant to relieve pain, instead amplify nociceptive signals through altered central nervous system processing. Understanding OIH is critical for clinicians to differentiate it from tolerance and to adjust therapy, potentially incorporating alternative analgesics or adjuvant treatments to mitigate this paradoxical hyperalgesia.
Neuropathic Pain and Hyperalgesia: Nerve Damage Examples
Neuropathic pain often manifests with hyperalgesia, an increased sensitivity to painful stimuli resulting from nerve damage. Common examples include diabetic neuropathy and postherpetic neuralgia, where damaged peripheral nerves cause exaggerated pain responses. These conditions highlight the critical role of nerve injury in amplifying pain perception beyond normal sensitivity thresholds.
Inflammatory Hyperalgesia: Pain Response in Chronic Inflammation
Inflammatory hyperalgesia, a heightened pain response caused by chronic inflammation, manifests when pro-inflammatory mediators such as prostaglandins and cytokines sensitize nociceptors at the injury site. This sensitization leads to exaggerated pain perception in conditions like rheumatoid arthritis and chronic inflammatory diseases. Persistent inflammation intensifies the release of substances that lower pain thresholds, resulting in increased sensitivity to both noxious and non-noxious stimuli.
Diabetic Neuropathy and Hyperalgesia: Sensory Changes Explained
Diabetic neuropathy exemplifies hyperalgesia through heightened pain sensitivity resulting from nerve damage caused by chronic high blood sugar levels. This condition disrupts normal sensory processing, leading to exaggerated pain signals in response to stimuli that are typically mildly painful or not painful at all. Understanding the sensory alterations in diabetic neuropathy aids in targeted pain management strategies for patients experiencing hyperalgesia.
Fibromyalgia: Widespread Hyperalgesia in Chronic Pain Syndromes
Fibromyalgia exemplifies widespread hyperalgesia, with patients experiencing heightened pain sensitivity across multiple body regions due to central nervous system sensitization. This chronic pain syndrome manifests as amplified pain signals, causing normally non-painful stimuli to be perceived as painful. Neuroimaging studies reveal alterations in pain processing pathways, underscoring the complex neurobiological mechanisms underlying fibromyalgia-associated hyperalgesia.
Migraine-Related Hyperalgesia: Heightened Sensitivity During Attacks
Migraine-related hyperalgesia manifests as an increased sensitivity to pain stimuli during migraine attacks, often causing normally non-painful sensations to become intensely painful. This heightened pain perception is linked to central sensitization within the trigeminovascular system, intensifying headache severity. Studies indicate that hyperalgesia contributes to the prolonged duration and increased frequency of migraine episodes, complicating treatment strategies.
Assessment and Diagnosis: Identifying Hyperalgesia in Patients
Assessment of hyperalgesia involves quantitative sensory testing (QST) to measure patients' pain thresholds and responses to typically non-painful stimuli. Clinicians utilize tools such as pressure algometers and thermal probes to identify heightened pain sensitivity, distinguishing hyperalgesia from other pain disorders. Accurate diagnosis requires correlating patient-reported symptoms with objective findings from sensory testing to tailor effective pain management strategies.
example of hyperalgesia in pain perception Infographic
 samplerz.com
samplerz.com