Psychoneuroimmunology explores the intricate relationship between the nervous system, immune response, and psychological factors in autoimmune disorders. In diseases like rheumatoid arthritis, stress and emotional health can significantly impact the immune system's ability to regulate inflammation. Research shows that psychological stress triggers the hypothalamic-pituitary-adrenal axis, leading to altered cytokine production and exacerbating autoimmune symptoms. Clinical studies reveal that patients with lupus often experience fluctuations in disease activity linked to mental health status. The interaction between neurotransmitters and immune cells highlights how depression or anxiety may worsen immune dysregulation. Understanding these neuroimmune pathways is crucial for developing integrated treatments that address both psychological and immunological aspects of autoimmune diseases.
Table of Comparison
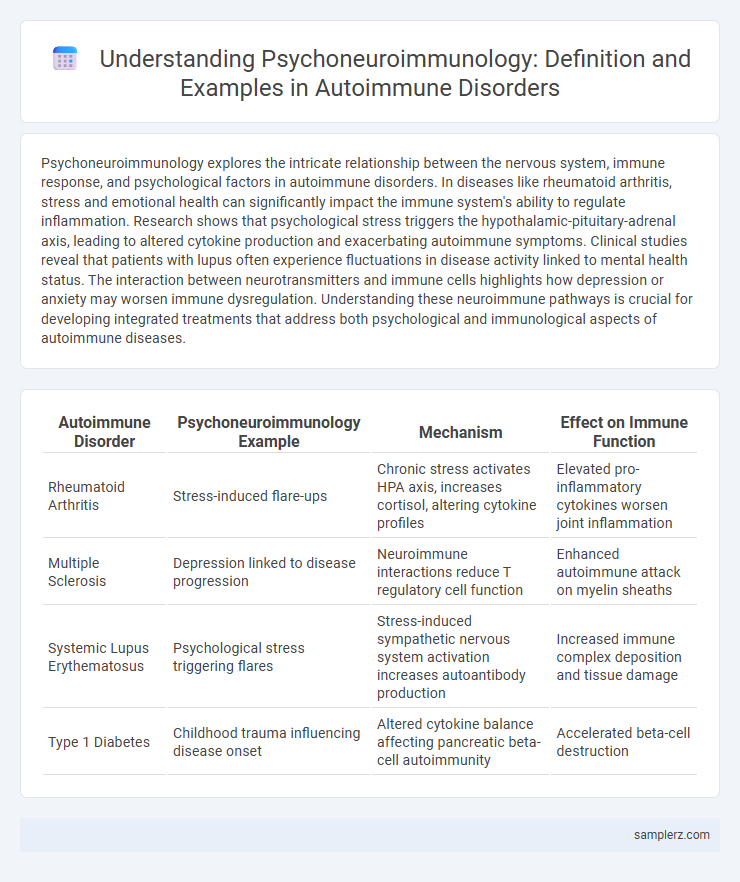
| Autoimmune Disorder | Psychoneuroimmunology Example | Mechanism | Effect on Immune Function |
|---|---|---|---|
| Rheumatoid Arthritis | Stress-induced flare-ups | Chronic stress activates HPA axis, increases cortisol, altering cytokine profiles | Elevated pro-inflammatory cytokines worsen joint inflammation |
| Multiple Sclerosis | Depression linked to disease progression | Neuroimmune interactions reduce T regulatory cell function | Enhanced autoimmune attack on myelin sheaths |
| Systemic Lupus Erythematosus | Psychological stress triggering flares | Stress-induced sympathetic nervous system activation increases autoantibody production | Increased immune complex deposition and tissue damage |
| Type 1 Diabetes | Childhood trauma influencing disease onset | Altered cytokine balance affecting pancreatic beta-cell autoimmunity | Accelerated beta-cell destruction |
Introduction to Psychoneuroimmunology and Autoimmune Disorders
Psychoneuroimmunology explores the complex interactions between the nervous, endocrine, and immune systems, particularly how psychological stress influences immune responses. In autoimmune disorders like rheumatoid arthritis and multiple sclerosis, psychoneuroimmunology reveals how chronic stress can exacerbate immune dysregulation, leading to increased inflammation and symptom severity. Understanding this interplay enhances therapeutic strategies that integrate psychological interventions to modulate immune function and improve patient outcomes.
How Stress Influences Autoimmune Disease Progression
Chronic stress triggers the release of cortisol and other stress hormones, which dysregulate immune cell function and increase inflammation, accelerating autoimmune disease progression. Psychoneuroimmunology studies reveal that stress-induced cytokine imbalances exacerbate conditions like rheumatoid arthritis and multiple sclerosis by promoting tissue damage. Effective stress management techniques can potentially modulate neuroimmune interactions, reducing flare-ups and improving patient outcomes in autoimmune disorders.
Case Study: Multiple Sclerosis and Mind-Body Interaction
Psychoneuroimmunology explores how stress and psychological factors influence immune function in autoimmune disorders like multiple sclerosis (MS). Case studies reveal that patients with MS experience fluctuations in symptom severity correlating with stress levels, suggesting a mind-body interaction affecting immune regulation. Therapeutic interventions targeting stress reduction, such as mindfulness and cognitive-behavioral therapy, show promise in modulating immune responses and improving quality of life for MS patients.
The Role of Depression in Rheumatoid Arthritis Flare-Ups
Depression significantly influences rheumatoid arthritis (RA) flare-ups by exacerbating systemic inflammation through altered cytokine production, particularly increased levels of interleukin-6 (IL-6) and tumor necrosis factor-alpha (TNF-a). Psychoneuroimmunology research highlights how stress-induced activation of the hypothalamic-pituitary-adrenal (HPA) axis impairs immune regulation, worsening joint inflammation and pain severity in RA patients. Therapeutic approaches targeting both depressive symptoms and inflammatory pathways have shown promise in reducing the frequency and intensity of RA exacerbations.
Psychosocial Factors Impacting Lupus Symptoms
Psychoneuroimmunology research highlights how psychosocial factors such as stress, depression, and social support directly influence lupus symptoms by modulating immune system activity and inflammatory responses. Studies show increased cortisol levels and altered cytokine profiles in lupus patients experiencing chronic stress, exacerbating disease flares and tissue damage. Targeted psychosocial interventions can improve immune regulation, reducing symptom severity and enhancing quality of life for individuals with lupus.
Mindfulness-Based Interventions in Autoimmune Conditions
Mindfulness-based interventions (MBIs) have shown promising effects on autoimmune disorders by modulating the psychoneuroimmunology pathways involved in disease progression. Studies reveal that MBIs reduce stress-related cortisol levels and inflammatory cytokines like IL-6 and TNF-alpha, which play key roles in autoimmune responses. These neuroimmune alterations contribute to symptom relief and improved quality of life in conditions such as rheumatoid arthritis and multiple sclerosis.
Neuroendocrine Pathways Linking Emotions and Immune Response
Neuroendocrine pathways involving the hypothalamic-pituitary-adrenal (HPA) axis critically link emotional stress to immune dysregulation in autoimmune disorders such as rheumatoid arthritis and multiple sclerosis. Cortisol secretion modulated by emotional states alters cytokine production, influencing inflammation and autoantibody activity. Understanding these mechanisms highlights the impact of psychological interventions on immune modulation and disease progression.
Childhood Trauma and Risk of Autoimmune Disease
Childhood trauma significantly increases the risk of developing autoimmune diseases through psychoneuroimmunology pathways, where early stress alters immune regulation and inflammatory responses. Research indicates that adverse childhood experiences (ACEs) correlate with heightened levels of pro-inflammatory cytokines and dysregulated hypothalamic-pituitary-adrenal (HPA) axis function, contributing to autoimmune pathogenesis. Understanding these mechanisms highlights the importance of addressing psychological stressors in preventing and managing autoimmune disorders.
Psychological Therapies Reducing Autoimmune Inflammation
Psychological therapies such as cognitive-behavioral therapy (CBT) and mindfulness-based stress reduction (MBSR) have demonstrated efficacy in lowering inflammation markers in autoimmune disorders like rheumatoid arthritis and lupus. These interventions modulate the neuroimmune axis by decreasing pro-inflammatory cytokines, including TNF-alpha and IL-6, thereby reducing disease activity. Clinical studies reveal that patients undergoing psychological therapy experience improved immune regulation and symptomatic relief, highlighting the integrative role of psychoneuroimmunology in autoimmune management.
Future Directions in Psychoneuroimmunology Research for Autoimmunity
Emerging research in psychoneuroimmunology highlights the potential of targeting stress-related neuroendocrine pathways to modulate immune responses in autoimmune disorders like rheumatoid arthritis and multiple sclerosis. Future investigations aim to integrate neuroimaging and molecular biomarkers to develop personalized interventions that reduce inflammation and improve clinical outcomes. Advances in understanding the gut-brain-immune axis could revolutionize therapeutic strategies by leveraging microbiome modulation to restore immune homeostasis in autoimmune patients.
example of psychoneuroimmunology in autoimmune disorder Infographic
 samplerz.com
samplerz.com