Steatorrhea is a clinical condition characterized by the presence of excess fat in stool, often indicating malabsorption in the gastrointestinal tract. A common example of steatorrhea in gastroenterology is chronic pancreatitis, where pancreatic enzyme deficiency disrupts fat digestion. This results in bulky, greasy, and foul-smelling stools that are typically difficult to flush. Celiac disease also presents with steatorrhea due to villous atrophy in the small intestine, leading to impaired nutrient absorption. In this condition, the immune response to gluten damages the intestinal lining, reducing fat absorption and causing fatty stools. Diagnostic tests such as stool fat analysis and serologic markers help confirm the presence of steatorrhea and its underlying cause.
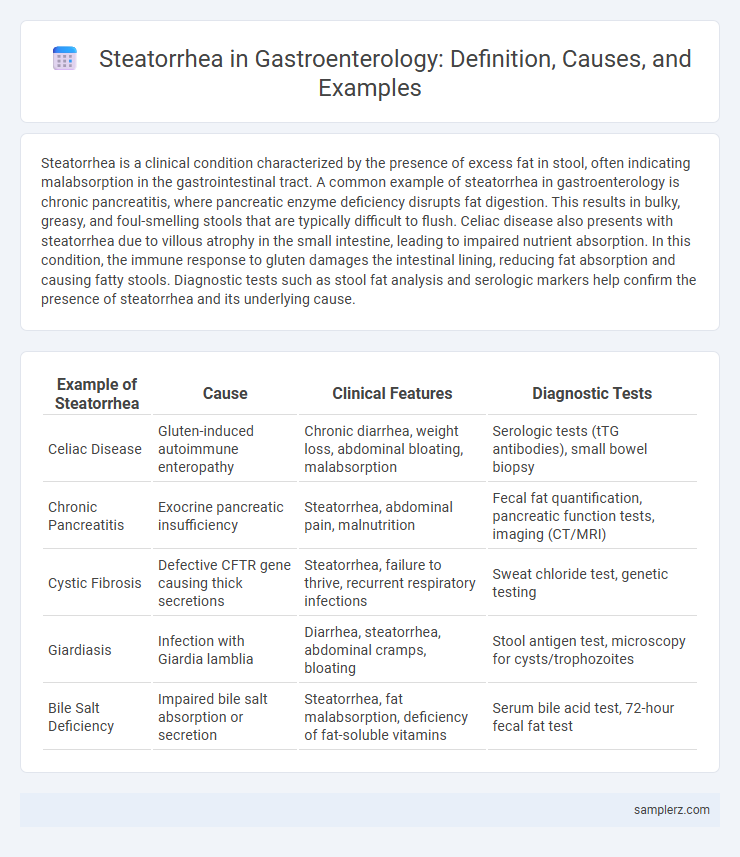
Table of Comparison
| Example of Steatorrhea | Cause | Clinical Features | Diagnostic Tests |
|---|---|---|---|
| Celiac Disease | Gluten-induced autoimmune enteropathy | Chronic diarrhea, weight loss, abdominal bloating, malabsorption | Serologic tests (tTG antibodies), small bowel biopsy |
| Chronic Pancreatitis | Exocrine pancreatic insufficiency | Steatorrhea, abdominal pain, malnutrition | Fecal fat quantification, pancreatic function tests, imaging (CT/MRI) |
| Cystic Fibrosis | Defective CFTR gene causing thick secretions | Steatorrhea, failure to thrive, recurrent respiratory infections | Sweat chloride test, genetic testing |
| Giardiasis | Infection with Giardia lamblia | Diarrhea, steatorrhea, abdominal cramps, bloating | Stool antigen test, microscopy for cysts/trophozoites |
| Bile Salt Deficiency | Impaired bile salt absorption or secretion | Steatorrhea, fat malabsorption, deficiency of fat-soluble vitamins | Serum bile acid test, 72-hour fecal fat test |
Understanding Steatorrhea: Definition and Overview
Steatorrhea is characterized by the presence of excess fat in stools, resulting in bulky, pale, and foul-smelling bowel movements that often float due to high fat content. This condition indicates malabsorption disorders such as chronic pancreatitis, celiac disease, or cystic fibrosis, where impaired digestion or absorption of dietary fats occurs. Accurate diagnosis involves stool fat analysis and evaluating underlying causes through pancreatic function tests and intestinal biopsies.
Common Causes of Steatorrhea in Gastroenterology
Steatorrhea, characterized by the presence of excess fat in stools, commonly arises from conditions impairing fat digestion or absorption such as chronic pancreatitis, celiac disease, and cystic fibrosis. Pancreatic enzyme insufficiency in chronic pancreatitis reduces lipase production, hindering fat breakdown, while intestinal mucosal damage in celiac disease disrupts nutrient absorption. Bile acid deficiency from cholestatic liver diseases also contributes by impairing micelle formation crucial for fat emulsification and absorption.
Classic Clinical Symptoms of Steatorrhea
Steatorrhea in gastroenterology typically presents with classic clinical symptoms such as bulky, pale, foul-smelling stools that are difficult to flush due to high fat content. Patients often experience oily or greasy stools accompanied by abdominal cramping, bloating, and weight loss from malabsorption. These manifestations indicate impaired fat digestion and absorption commonly associated with conditions like chronic pancreatitis or celiac disease.
Steatorrhea in Celiac Disease: A Hallmark Symptom
Steatorrhea in celiac disease occurs due to malabsorption caused by villous atrophy in the small intestine, leading to excess fat in stools that appear bulky, pale, and foul-smelling. This hallmark symptom is a direct result of impaired digestion and absorption of dietary fats, often accompanied by other signs such as weight loss and nutrient deficiencies. Diagnosis relies on serologic testing and intestinal biopsy, with a gluten-free diet serving as the primary treatment to restore intestinal mucosa and reduce steatorrhea.
Chronic Pancreatitis as a Source of Steatorrhea
Chronic pancreatitis leads to steatorrhea due to the pancreas's diminished ability to produce digestive enzymes, particularly lipase, which impairs fat digestion and absorption. This malabsorption results in fatty, foul-smelling stools characteristic of steatorrhea. Diagnosing steatorrhea in chronic pancreatitis involves stool fat quantification and imaging studies like CT or MRI to assess pancreatic damage.
Cystic Fibrosis and Pancreatic Exocrine Insufficiency
Steatorrhea in gastroenterology commonly presents in patients with Cystic Fibrosis due to thickened secretions obstructing pancreatic ducts, leading to malabsorption of fats. Pancreatic Exocrine Insufficiency, often secondary to chronic pancreatitis or Cystic Fibrosis, results in insufficient secretion of digestive enzymes, causing oily, foul-smelling stools characteristic of steatorrhea. Effective diagnosis involves quantitative fecal fat testing and measurement of pancreatic enzyme levels to guide enzyme replacement therapy.
Steatorrhea in Small Intestinal Bacterial Overgrowth (SIBO)
Steatorrhea in Small Intestinal Bacterial Overgrowth (SIBO) results from excessive bacterial fermentation that impairs fat absorption, leading to greasy, foul-smelling stools rich in fat content. This condition disrupts normal digestion as bacteria deconjugate bile acids, reducing micelle formation necessary for lipid emulsification. Diagnosing SIBO-related steatorrhea involves breath tests for hydrogen and methane and stool fat quantification to guide targeted antibiotic and dietary therapy.
Diagnostic Approaches for Detecting Steatorrhea
Quantitative fecal fat analysis remains the gold standard for diagnosing steatorrhea, requiring collection of stool samples over 72 hours to measure fat content exceeding 7 grams per day. Magnetic resonance imaging (MRI) and endoscopic ultrasound can help identify underlying pancreatic disorders contributing to malabsorption. Breath tests, such as the 13C-mixed triglyceride breath test, offer non-invasive evaluation of pancreatic exocrine function aiding in early detection of steatorrhea-related conditions.
Dietary and Lifestyle Modifications for Managing Steatorrhea
Dietary and lifestyle modifications play a crucial role in managing steatorrhea by reducing fat malabsorption and improving nutrient absorption. A low-fat diet with medium-chain triglycerides (MCT) helps decrease fat content in stools while supplementing fat-soluble vitamins A, D, E, and K addresses deficiencies. Regularly monitoring pancreatic enzyme supplementation and avoiding alcohol or smoking can enhance digestive function and reduce symptom severity in patients with chronic pancreatitis or cystic fibrosis-related steatorrhea.
Prognosis and Long-Term Monitoring of Steatorrhea in Gastroenterology
Steatorrhea, characterized by excessive fat in stools, often indicates malabsorption disorders such as chronic pancreatitis or celiac disease. Prognosis depends on identifying and managing the underlying cause, with untreated conditions potentially leading to malnutrition and vitamin deficiencies. Long-term monitoring includes regular assessment of nutritional status, pancreatic function tests, and adherence to dietary modifications to prevent complications.
example of steatorrhea in gastroenterology Infographic
 samplerz.com
samplerz.com