Ascites is a common complication in patients with cirrhosis, characterized by the accumulation of fluid in the abdominal cavity. This condition occurs due to increased pressure in the portal vein and decreased liver function, leading to fluid leakage from blood vessels. Data indicates that nearly 60% of cirrhosis patients develop ascites within ten years of diagnosis, impacting overall morbidity and quality of life. The clinical presentation of ascites in cirrhosis includes abdominal distension, discomfort, and weight gain. Diagnostic methods involve physical examination and imaging techniques such as ultrasound to quantify fluid volume. Management strategies focus on sodium restriction, diuretics, and in severe cases, paracentesis or transjugular intrahepatic portosystemic shunt (TIPS) to reduce portal pressure and control fluid accumulation.
Table of Comparison
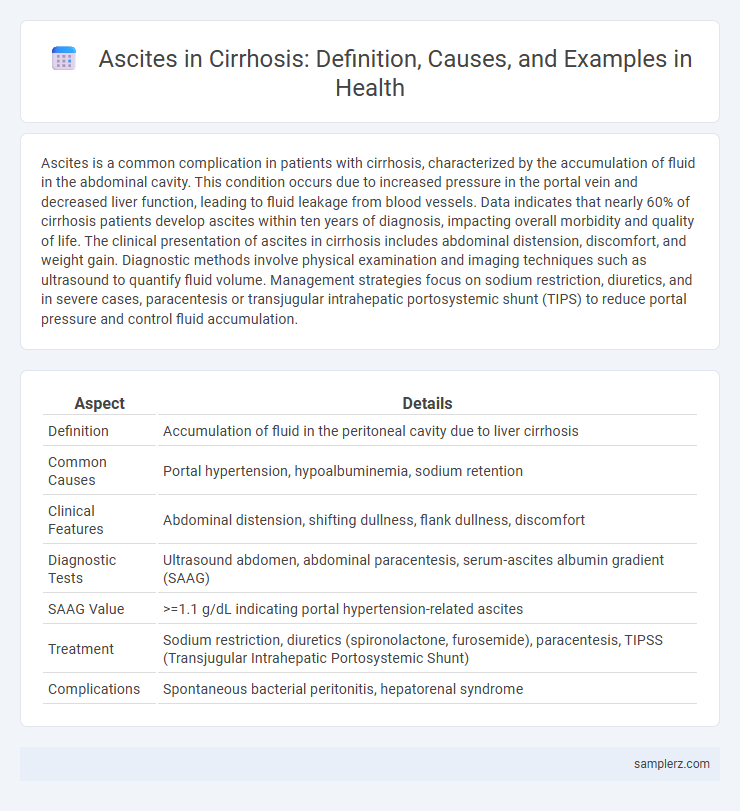
| Aspect | Details |
|---|---|
| Definition | Accumulation of fluid in the peritoneal cavity due to liver cirrhosis |
| Common Causes | Portal hypertension, hypoalbuminemia, sodium retention |
| Clinical Features | Abdominal distension, shifting dullness, flank dullness, discomfort |
| Diagnostic Tests | Ultrasound abdomen, abdominal paracentesis, serum-ascites albumin gradient (SAAG) |
| SAAG Value | >=1.1 g/dL indicating portal hypertension-related ascites |
| Treatment | Sodium restriction, diuretics (spironolactone, furosemide), paracentesis, TIPSS (Transjugular Intrahepatic Portosystemic Shunt) |
| Complications | Spontaneous bacterial peritonitis, hepatorenal syndrome |
Understanding Ascites in Liver Cirrhosis
Ascites in liver cirrhosis results from portal hypertension and hypoalbuminemia, causing fluid accumulation in the peritoneal cavity. Common signs include abdominal distension, discomfort, and shifting dullness on physical examination. Management relies on sodium restriction, diuretics, and therapeutic paracentesis to alleviate symptoms and prevent complications such as spontaneous bacterial peritonitis.
Pathophysiology: How Cirrhosis Leads to Ascites
Cirrhosis causes scarring and nodular regeneration in the liver, leading to increased resistance to portal blood flow and resulting in portal hypertension. Elevated portal pressure triggers splanchnic vasodilation and sodium retention by the kidneys, promoting fluid accumulation in the peritoneal cavity. Hypoalbuminemia from impaired hepatic synthesis further reduces plasma oncotic pressure, exacerbating the transudation of fluid and formation of ascites.
Common Signs and Symptoms of Ascites
Ascites in cirrhosis commonly presents with abdominal distension due to fluid accumulation, often accompanied by discomfort or a feeling of fullness. Patients may experience weight gain and swelling in the lower extremities from fluid retention. Other symptoms include shortness of breath caused by increased abdominal pressure on the diaphragm and reduced lung capacity.
Diagnostic Criteria for Ascites in Cirrhosis
Diagnostic criteria for ascites in cirrhosis include clinical evidence such as abdominal distension and fluid wave, confirmed by ultrasonography showing free peritoneal fluid. Paracentesis analysis reveals a serum-ascites albumin gradient (SAAG) greater than 1.1 g/dL, indicating portal hypertension as the underlying cause. Additional laboratory tests assess total protein concentration and exclude infections, guiding appropriate management strategies.
Case Study: Classic Example of Ascites in Cirrhotic Patient
A classic case study of ascites in a cirrhotic patient involves a 56-year-old male with alcoholic liver cirrhosis presenting with abdominal distension, peripheral edema, and dyspnea due to large-volume ascitic fluid accumulation. Diagnostic paracentesis revealed a high serum-ascites albumin gradient (SAAG) above 1.1 g/dL, confirming portal hypertension as the underlying cause. Management included sodium restriction, diuretics like spironolactone and furosemide, and serial paracentesis to alleviate symptoms and prevent complications such as spontaneous bacterial peritonitis.
Laboratory and Imaging Findings in Cirrhotic Ascites
Laboratory findings in cirrhotic ascites typically reveal low serum albumin levels and an elevated serum-ascites albumin gradient (SAAG) greater than 1.1 g/dL, confirming portal hypertension as the underlying cause. Imaging studies, including abdominal ultrasound, often demonstrate the presence of free fluid in the peritoneal cavity along with features of cirrhosis such as a nodular liver surface and splenomegaly. Doppler ultrasound may also be used to assess portal vein patency and flow abnormalities associated with cirrhosis.
Risk Factors for Developing Ascites in Cirrhosis
Chronic liver diseases such as hepatitis C and alcoholic liver disease significantly increase the risk of developing ascites in cirrhosis patients. Portal hypertension and hypoalbuminemia contribute to fluid accumulation in the peritoneal cavity, exacerbating ascites. Advanced age, male gender, and ongoing alcohol consumption further elevate the likelihood of ascites formation in cirrhotic individuals.
Complications Associated with Ascites in Cirrhosis
Ascites in cirrhosis commonly leads to complications such as spontaneous bacterial peritonitis (SBP), hepatorenal syndrome, and respiratory distress due to diaphragmatic elevation. The accumulation of fluid increases intra-abdominal pressure, which can cause abdominal pain, bacterial infections, and impair kidney function, significantly worsening patient prognosis. Management of these complications requires timely intervention with antibiotics, diuretics, and sometimes paracentesis to prevent further morbidity and mortality.
Therapeutic Approaches to Managing Ascites
Therapeutic approaches to managing ascites in cirrhosis primarily include sodium restriction and diuretic therapy, with spironolactone and furosemide as first-line medications to promote fluid excretion. In refractory cases, large-volume paracentesis offers symptomatic relief and reduces abdominal pressure, while transjugular intrahepatic portosystemic shunt (TIPS) may be considered to decrease portal hypertension. Monitoring renal function and electrolyte balance is crucial to prevent complications during treatment.
Preventive Strategies for Ascites in Patients with Cirrhosis
Preventive strategies for ascites in patients with cirrhosis emphasize sodium restriction to less than 2 grams per day and the use of diuretics such as spironolactone and furosemide for fluid balance control. Regular monitoring of body weight and abdominal girth helps detect early fluid accumulation, allowing timely intervention. Avoidance of alcohol and prompt management of underlying liver disease also play crucial roles in reducing ascites risk.
example of ascites in cirrhosis Infographic
 samplerz.com
samplerz.com