Atrial flutter is a type of cardiac arrhythmia characterized by rapid, regular atrial contractions occurring at rates typically between 240 and 400 beats per minute. This condition results from a reentrant circuit in the right atrium, leading to a sawtooth pattern on the electrocardiogram (ECG). The irregular atrial rhythm causes inefficient blood flow, which can increase the risk of stroke and heart failure if left untreated. Patients with atrial flutter often present symptoms such as palpitations, shortness of breath, dizziness, and fatigue. Diagnosis relies on ECG findings that demonstrate characteristic flutter waves, often best seen in leads II, III, and aVF. Treatment options include catheter ablation to target the reentrant pathway, rate control medications, and anticoagulation therapy to prevent thromboembolic events.
Table of Comparison
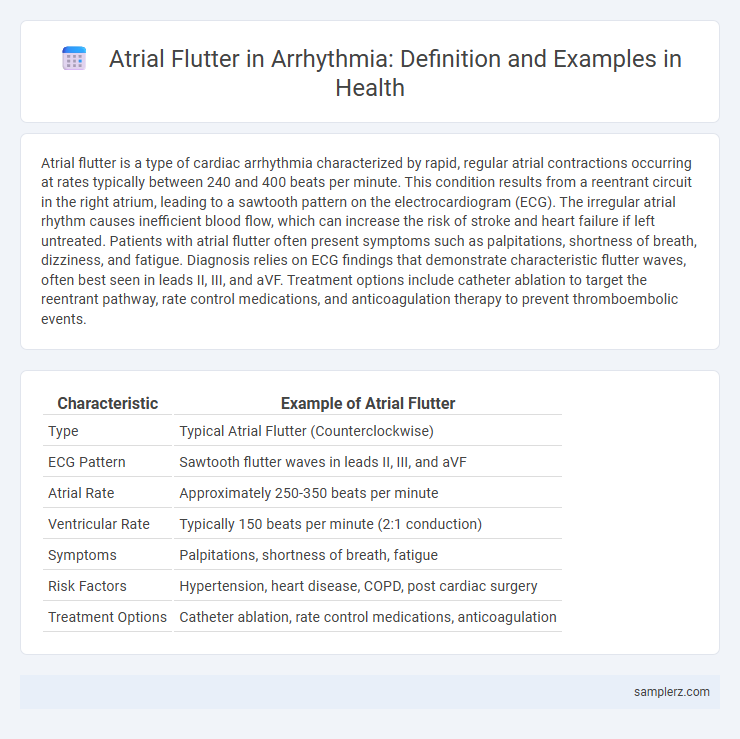
| Characteristic | Example of Atrial Flutter |
|---|---|
| Type | Typical Atrial Flutter (Counterclockwise) |
| ECG Pattern | Sawtooth flutter waves in leads II, III, and aVF |
| Atrial Rate | Approximately 250-350 beats per minute |
| Ventricular Rate | Typically 150 beats per minute (2:1 conduction) |
| Symptoms | Palpitations, shortness of breath, fatigue |
| Risk Factors | Hypertension, heart disease, COPD, post cardiac surgery |
| Treatment Options | Catheter ablation, rate control medications, anticoagulation |
Understanding Atrial Flutter: A Common Cardiac Arrhythmia
Atrial flutter is characterized by rapid, regular atrial contractions typically around 250-350 beats per minute, leading to a distinct sawtooth pattern on an electrocardiogram (ECG). This arrhythmia originates from a reentrant circuit in the right atrium, causing inefficient atrial contractions and potential complications such as stroke or heart failure. Understanding atrial flutter is crucial for accurate diagnosis and effective management, often involving rate control, rhythm conversion, or catheter ablation to restore normal sinus rhythm.
Key Symptoms of Atrial Flutter in Patients
Atrial flutter in arrhythmia commonly presents with rapid, regular heartbeats typically ranging from 150 to 250 beats per minute. Patients often experience palpitations, shortness of breath, and episodes of dizziness or lightheadedness due to decreased cardiac output. Fatigue and chest discomfort may also be reported, highlighting the need for timely diagnosis and management.
Causes and Risk Factors for Developing Atrial Flutter
Atrial flutter is often caused by structural heart abnormalities such as cardiomyopathy, previous myocardial infarction, or significant atrial scarring. Key risk factors include hypertension, chronic obstructive pulmonary disease (COPD), and hyperthyroidism, which contribute to electrical instability in the atria. Patients with a history of atrial fibrillation or those undergoing cardiac surgery also face an increased likelihood of developing atrial flutter.
How Atrial Flutter Differs from Other Arrhythmias
Atrial flutter is characterized by a rapid but regular atrial rhythm, typically around 250-350 beats per minute, distinguishing it from atrial fibrillation, which presents with irregular and often faster atrial rates. Unlike ventricular arrhythmias, atrial flutter primarily affects the atria, resulting in a sawtooth pattern on an electrocardiogram (ECG) that is diagnostic of this specific arrhythmia. The organized electrical circuit in atrial flutter contrasts with the chaotic signals seen in other supraventricular arrhythmias, leading to distinct clinical and treatment implications.
Diagnostic Approaches for Detecting Atrial Flutter
Electrocardiogram (ECG) remains the primary diagnostic tool for detecting atrial flutter, characterized by sawtooth flutter waves predominantly in leads II, III, and aVF. Holter monitoring enhances detection of intermittent atrial flutter episodes by providing continuous rhythm analysis over 24 to 48 hours. Advanced methods like electrophysiological studies offer precise mapping of atrial circuits, facilitating targeted ablation therapy.
Electrocardiogram (ECG) Findings in Atrial Flutter
Atrial flutter presents on an electrocardiogram (ECG) with a characteristic sawtooth pattern of flutter waves, especially visible in leads II, III, and aVF, indicating rapid atrial depolarization typically around 250-350 beats per minute. The ventricular response often appears regular or variable depending on the conduction ratio, commonly 2:1 block generating a ventricular rate near 150 beats per minute. Distinct absence of distinct P waves and presence of consistent atrial flutter waves differentiate atrial flutter from other arrhythmias such as atrial fibrillation.
Real-Life Case Example: Presentation of Atrial Flutter
A 65-year-old male with a history of hypertension presented to the emergency department with palpitations, shortness of breath, and dizziness; an electrocardiogram (ECG) revealed a classic sawtooth pattern indicative of atrial flutter. The patient exhibited an atrial rate of approximately 300 beats per minute with variable ventricular response, confirming the diagnosis. Timely intervention with rate control medications and consideration for catheter ablation was initiated to manage this arrhythmia and prevent complications such as stroke.
Management and Treatment Options for Atrial Flutter
Management of atrial flutter involves rate control using beta-blockers or calcium channel blockers to prevent rapid ventricular response, alongside anticoagulation therapy to reduce stroke risk. Catheter ablation targeting the cavotricuspid isthmus is highly effective in restoring normal rhythm and preventing recurrence. In cases where ablation is not feasible, antiarrhythmic drugs such as amiodarone may be prescribed to maintain sinus rhythm and improve patient outcomes.
Potential Complications Associated with Atrial Flutter
Atrial flutter, a type of arrhythmia characterized by rapid and regular atrial contractions, poses significant risks including increased likelihood of stroke due to blood clot formation in the atria. Potential complications also encompass heart failure from inefficient cardiac output and the development of tachycardia-induced cardiomyopathy if left untreated. Early diagnosis and management are critical to preventing these serious outcomes associated with atrial flutter.
Prevention and Long-Term Outlook for Atrial Flutter Patients
Preventing atrial flutter involves managing risk factors such as high blood pressure, obesity, and excessive alcohol consumption through lifestyle changes and medication adherence. Long-term outlook for atrial flutter patients improves significantly with early diagnosis, regular monitoring, and treatments like catheter ablation, which restores normal heart rhythm and reduces stroke risk. Consistent control of underlying conditions and follow-up care are essential to prevent recurrence and ensure optimal heart health.
example of atrial flutter in arrhythmia Infographic
 samplerz.com
samplerz.com