Comorbidity in psychiatry refers to the co-occurrence of two or more psychiatric disorders within the same individual. A common example is the presence of major depressive disorder alongside generalized anxiety disorder. Data from clinical studies indicate that nearly 60% of patients diagnosed with depression also exhibit symptoms of anxiety, highlighting the frequent overlap between these conditions. Another prevalent example of psychiatric comorbidity is the co-occurrence of substance use disorders with bipolar disorder. Research shows that approximately 45% of individuals with bipolar disorder struggle with alcohol or drug abuse, complicating treatment outcomes. This data emphasizes the need for integrated treatment approaches that address both mood instability and substance dependency simultaneously.
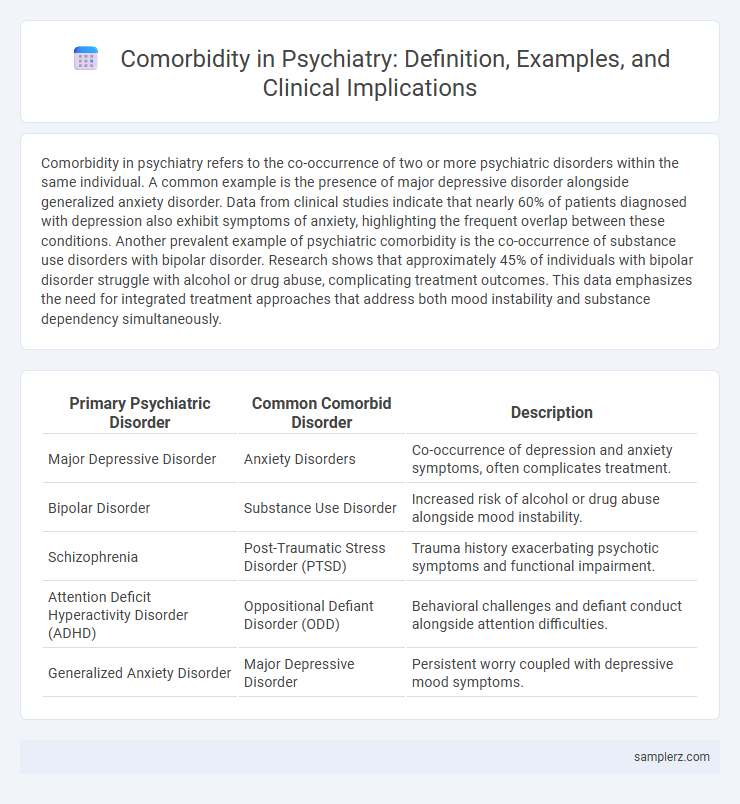
Table of Comparison
| Primary Psychiatric Disorder | Common Comorbid Disorder | Description |
|---|---|---|
| Major Depressive Disorder | Anxiety Disorders | Co-occurrence of depression and anxiety symptoms, often complicates treatment. |
| Bipolar Disorder | Substance Use Disorder | Increased risk of alcohol or drug abuse alongside mood instability. |
| Schizophrenia | Post-Traumatic Stress Disorder (PTSD) | Trauma history exacerbating psychotic symptoms and functional impairment. |
| Attention Deficit Hyperactivity Disorder (ADHD) | Oppositional Defiant Disorder (ODD) | Behavioral challenges and defiant conduct alongside attention difficulties. |
| Generalized Anxiety Disorder | Major Depressive Disorder | Persistent worry coupled with depressive mood symptoms. |
Overview of Psychiatric Comorbidity
Psychiatric comorbidity frequently involves the simultaneous presence of major depressive disorder and generalized anxiety disorder, complicating diagnosis and treatment. Substance use disorders often co-occur with mood disorders, exacerbating symptom severity and increasing the risk of chronic relapse. Understanding these coexisting psychiatric conditions is crucial for developing integrated treatment plans that address multiple disorders concurrently.
Common Comorbid Disorders in Psychiatry
Depression and anxiety disorders frequently co-occur, with studies indicating that nearly 60% of individuals diagnosed with major depressive disorder also experience an anxiety disorder. Substance use disorders often complicate psychiatric treatment, as coexisting addiction can exacerbate symptoms of bipolar disorder and schizophrenia. Post-traumatic stress disorder (PTSD) commonly appears alongside depression and substance misuse, creating a complex clinical profile that requires integrated therapeutic approaches.
Depression and Anxiety: A Frequent Comorbidity
Depression and anxiety frequently co-occur, with studies indicating that up to 60% of patients diagnosed with major depressive disorder also experience an anxiety disorder. This comorbidity complicates diagnosis and treatment, often requiring integrated therapeutic approaches targeting both mood and anxiety symptoms. Understanding the high prevalence of depression-anxiety comorbidity enhances clinical management and improves patient outcomes in psychiatric practice.
Bipolar Disorder with Substance Use Disorders
Bipolar Disorder frequently co-occurs with Substance Use Disorders, complicating diagnosis and treatment due to overlapping symptoms such as mood swings and impaired judgment. Patients with this comorbidity often experience increased risk of hospitalization, poorer medication adherence, and higher rates of relapse. Effective management requires integrated clinical approaches targeting both mood stabilization and substance abuse interventions.
Schizophrenia and Obsessive-Compulsive Symptoms
Schizophrenia frequently presents comorbid Obsessive-Compulsive Symptoms (OCS), complicating diagnosis and treatment outcomes. Studies show that approximately 30% of patients with schizophrenia exhibit OCS, leading to increased severity of psychotic symptoms and higher functional impairment. Effective management requires integrated psychiatric approaches combining antipsychotic and selective serotonin reuptake inhibitors (SSRIs) therapies to address both symptom domains.
ADHD and Oppositional Defiant Disorder
Attention Deficit Hyperactivity Disorder (ADHD) frequently co-occurs with Oppositional Defiant Disorder (ODD), representing a common psychiatric comorbidity in children and adolescents. This combination exacerbates challenges such as impulsivity, irritability, and defiant behaviors, complicating diagnosis and treatment strategies. Understanding the overlapping symptoms of ADHD and ODD is crucial for effective behavioral interventions and medication management in mental health care.
Eating Disorders and Mood Disorders
Eating disorders such as anorexia nervosa and bulimia nervosa frequently co-occur with mood disorders, including major depressive disorder and bipolar disorder, complicating diagnosis and treatment approaches. Studies show that approximately 30-50% of individuals with eating disorders also meet criteria for a mood disorder, highlighting the need for integrated psychiatric care. Effective management requires addressing both the psychological aspects of mood disturbances and the behavioral symptoms of eating disorders to improve overall patient outcomes.
PTSD with Co-occurring Depression
PTSD frequently co-occurs with depression, creating a complex clinical presentation that intensifies symptom severity and complicates treatment strategies. Epidemiological studies show up to 50% of individuals with PTSD also meet criteria for major depressive disorder, highlighting significant comorbidity. This dual diagnosis demands integrated therapeutic approaches to address overlapping symptoms and improve patient outcomes.
Personality Disorders and Comorbidity Patterns
Personality disorders frequently exhibit complex comorbidity patterns, often co-occurring with mood disorders such as major depressive disorder or anxiety disorders, complicating diagnosis and treatment. Borderline personality disorder, for example, commonly presents alongside substance use disorders, post-traumatic stress disorder, and eating disorders, indicating overlapping etiological factors. Recognizing these comorbidities is essential in psychiatry to tailor integrated therapeutic approaches and improve patient outcomes.
Impact of Comorbidity on Treatment Outcomes
Comorbidity in psychiatry, such as the coexistence of major depressive disorder and generalized anxiety disorder, significantly complicates treatment effectiveness by increasing symptom severity and prolonging recovery time. Patients with dual diagnoses often require integrated therapeutic approaches, combining pharmacotherapy and psychotherapy tailored to address both conditions simultaneously. This complexity can lead to higher rates of treatment resistance, poorer adherence, and increased risk of relapse, underscoring the urgent need for specialized care protocols.
example of comorbidity in psychiatry Infographic
 samplerz.com
samplerz.com