Iatrogenesis in surgery refers to unintended harm caused by medical intervention during surgical procedures. An example includes postoperative infections resulting from inadequate sterile techniques in the operating room. These infections can lead to prolonged hospital stays, increased healthcare costs, and serious complications such as sepsis. Another instance of iatrogenesis is nerve damage occurring during the removal of a tumor or organ. Surgical instruments may inadvertently injure adjacent nerves, causing loss of sensation or motor function. Monitoring surgical precision and implementing advanced imaging techniques are critical in minimizing such risks and improving patient outcomes.
Table of Comparison
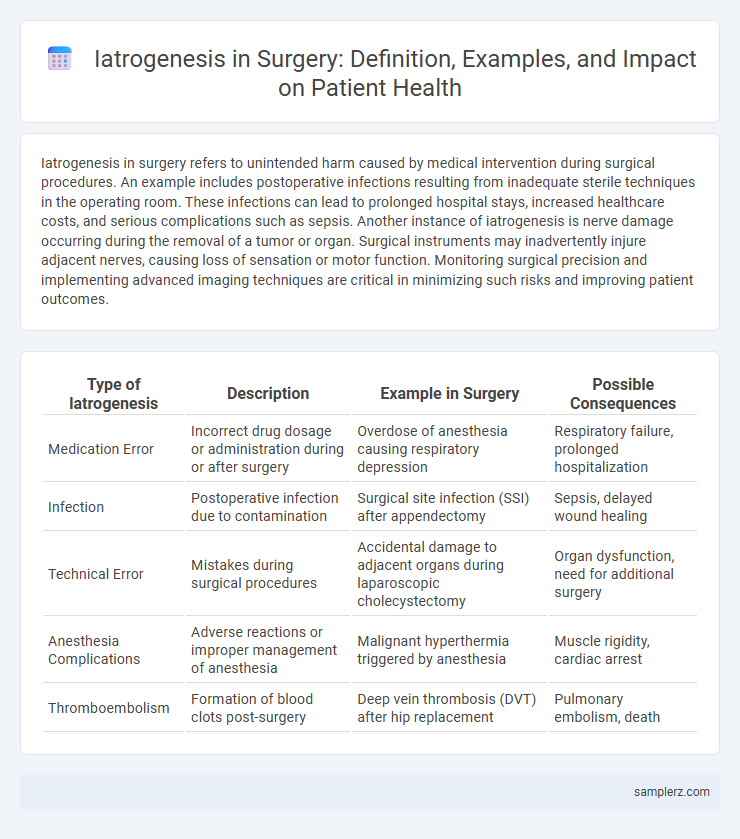
| Type of Iatrogenesis | Description | Example in Surgery | Possible Consequences |
|---|---|---|---|
| Medication Error | Incorrect drug dosage or administration during or after surgery | Overdose of anesthesia causing respiratory depression | Respiratory failure, prolonged hospitalization |
| Infection | Postoperative infection due to contamination | Surgical site infection (SSI) after appendectomy | Sepsis, delayed wound healing |
| Technical Error | Mistakes during surgical procedures | Accidental damage to adjacent organs during laparoscopic cholecystectomy | Organ dysfunction, need for additional surgery |
| Anesthesia Complications | Adverse reactions or improper management of anesthesia | Malignant hyperthermia triggered by anesthesia | Muscle rigidity, cardiac arrest |
| Thromboembolism | Formation of blood clots post-surgery | Deep vein thrombosis (DVT) after hip replacement | Pulmonary embolism, death |
Common Surgical Procedures Leading to Iatrogenesis
Common surgical procedures such as appendectomies, cholecystectomies, and orthopedic surgeries frequently lead to iatrogenesis due to complications like infections, nerve damage, or anesthesia-related issues. Postoperative infections in cesarean sections and laparotomies remain significant contributors to iatrogenic harm. Surgeons must prioritize sterile techniques and vigilant postoperative monitoring to reduce the incidence of these adverse events.
Case Studies: Iatrogenic Injuries During Surgery
Case studies of iatrogenic injuries during surgery highlight instances such as accidental nerve damage during thyroidectomy, resulting in vocal cord paralysis, and unintentional bowel perforation in laparoscopic procedures causing peritonitis. These cases underscore the critical need for precise surgical technique and thorough preoperative planning to minimize harm. Data from multiple hospital audits reveal that careful intraoperative monitoring and prompt postoperative intervention significantly reduce the severity of adverse iatrogenic outcomes.
Postoperative Complications as Iatrogenic Outcomes
Postoperative complications such as surgical site infections, hemorrhage, and deep vein thrombosis exemplify iatrogenesis resulting directly from surgical interventions. These adverse outcomes often stem from factors like improper aseptic techniques, inadequate hemostasis, or prolonged immobilization during recovery. Understanding and mitigating these risks through improved surgical protocols and patient monitoring is essential to reduce iatrogenic harm in surgical care.
Surgical Errors: Unintended Consequences for Patients
Surgical errors represent a significant cause of iatrogenesis, leading to unintended patient outcomes such as infections, organ damage, or anesthesia complications. Misidentification of surgical sites and accidental nerve injury remain prevalent causes of postoperative morbidity. Implementing strict surgical checklists and advanced intraoperative monitoring can significantly reduce these iatrogenic risks and enhance patient safety outcomes.
Medication-Related Iatrogenesis in the Operating Room
Medication-related iatrogenesis in the operating room often occurs due to anesthetic complications, such as overdose or allergic reactions to neuromuscular blockers and opioids. Errors in drug administration, including incorrect dosing or timing of prophylactic antibiotics, can lead to adverse outcomes like surgical site infections or hemodynamic instability. Monitoring protocols and standardized medication checks are critical to minimizing these preventable medication-related surgical complications.
Iatrogenic Infections Arising from Surgical Interventions
Iatrogenic infections arising from surgical interventions often result from contamination during operative procedures, including the introduction of bacteria into sterile body cavities. Common examples include surgical site infections (SSIs), which can lead to complications such as abscesses, sepsis, or delayed wound healing. Preventive measures like strict aseptic techniques and prophylactic antibiotic administration are critical to minimizing the incidence of these healthcare-associated infections.
Device-Related Iatrogenic Events in Surgery
Device-related iatrogenic events in surgery often involve complications such as retained surgical instruments, malfunctioning implants, or improper device placement leading to tissue damage. Examples include nerve injury from surgical retractors, infection caused by contaminated surgical instruments, and implant failure causing postoperative pain or impaired function. Addressing these risks requires strict adherence to surgical protocols and advanced monitoring of device integrity throughout the procedure.
Strategies to Prevent Iatrogenesis in Surgical Practice
Implementing evidence-based surgical protocols significantly reduces the risk of iatrogenic complications such as inadvertent nerve damage or postoperative infections. Strict adherence to sterilization techniques, surgical checklists like the WHO Surgical Safety Checklist, and continuous team training enhance patient safety during operative procedures. Preoperative planning using advanced imaging and real-time intraoperative monitoring further minimizes surgical errors, promoting optimal patient outcomes.
Recognizing and Managing Iatrogenic Surgical Complications
Iatrogenic surgical complications commonly include infections, nerve injuries, and organ damage caused unintentionally during procedures. Early recognition through vigilant monitoring of symptoms such as unexpected pain, fever, or functional impairment is critical for timely intervention. Effective management involves prompt diagnostic imaging, surgical revision if necessary, and targeted antibiotic therapy to reduce morbidity and improve patient outcomes.
Patient Safety Protocols to Minimize Surgical Iatrogenesis
Surgical iatrogenesis, such as postoperative infections and inadvertent organ damage, can be significantly reduced through strict adherence to patient safety protocols including surgical checklists, sterile techniques, and preoperative verification processes. Implementing standardized safety measures like time-outs and comprehensive staff training enhances communication and error prevention in the operating room. Continuous monitoring and adherence to these protocols are critical in minimizing adverse events and improving surgical outcomes.
example of iatrogenesis in surgery Infographic
 samplerz.com
samplerz.com