Cyanosis is a clinical sign characterized by a bluish discoloration of the skin and mucous membranes due to low oxygen levels in the blood. In pulmonology, cyanosis commonly appears in conditions such as chronic obstructive pulmonary disease (COPD) and pulmonary embolism, where impaired lung function disrupts oxygen exchange. This visible symptom indicates hypoxemia, which requires prompt evaluation and intervention to prevent tissue damage. In cases of pneumonia, cyanosis may develop as inflammation and fluid accumulation limit oxygenation in the alveoli. Patients with congenital heart defects like Tetralogy of Fallot also present cyanosis due to abnormal blood flow causing decreased oxygen saturation. Monitoring oxygen levels with pulse oximetry and arterial blood gas analysis is essential in managing cyanosis in pulmonary diseases.
Table of Comparison
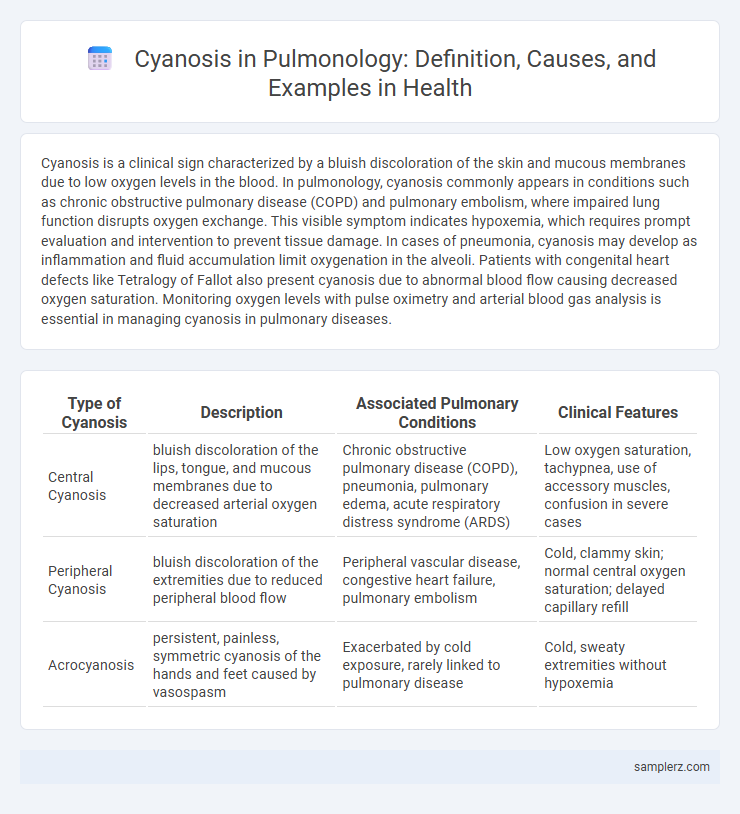
| Type of Cyanosis | Description | Associated Pulmonary Conditions | Clinical Features |
|---|---|---|---|
| Central Cyanosis | bluish discoloration of the lips, tongue, and mucous membranes due to decreased arterial oxygen saturation | Chronic obstructive pulmonary disease (COPD), pneumonia, pulmonary edema, acute respiratory distress syndrome (ARDS) | Low oxygen saturation, tachypnea, use of accessory muscles, confusion in severe cases |
| Peripheral Cyanosis | bluish discoloration of the extremities due to reduced peripheral blood flow | Peripheral vascular disease, congestive heart failure, pulmonary embolism | Cold, clammy skin; normal central oxygen saturation; delayed capillary refill |
| Acrocyanosis | persistent, painless, symmetric cyanosis of the hands and feet caused by vasospasm | Exacerbated by cold exposure, rarely linked to pulmonary disease | Cold, sweaty extremities without hypoxemia |
Understanding Cyanosis: Definition and Significance in Pulmonology
Cyanosis in pulmonology refers to the bluish discoloration of the skin and mucous membranes due to insufficient oxygen saturation in the blood, typically below 85%. It signifies underlying respiratory or cardiovascular conditions such as chronic obstructive pulmonary disease (COPD), pulmonary embolism, or congenital heart defects that impair oxygen delivery. Early recognition of central cyanosis is critical for diagnosing hypoxemia and guiding appropriate interventions in patients with compromised pulmonary function.
Common Pulmonary Causes of Cyanosis
Cyanosis commonly arises in pulmonology due to conditions causing impaired oxygenation, such as chronic obstructive pulmonary disease (COPD), pneumonia, and pulmonary embolism. These disorders lead to inadequate oxygen exchange in the lungs, resulting in reduced arterial oxygen saturation visible as bluish discoloration of the skin and mucous membranes. Early identification of hypoxemia in these pulmonary diseases is crucial for effective management and preventing severe tissue hypoxia.
Central Cyanosis: Clinical Examples in Respiratory Disorders
Central cyanosis in pulmonology often presents in conditions such as chronic obstructive pulmonary disease (COPD), pulmonary edema, and severe pneumonia, where impaired oxygenation leads to a bluish discoloration of the tongue and mucous membranes. In interstitial lung diseases like idiopathic pulmonary fibrosis, reduced alveolar oxygen exchange causes central cyanosis due to hypoxemia. Acute respiratory distress syndrome (ARDS) can also manifest with central cyanosis, reflecting critical impairment in pulmonary gas exchange.
Peripheral Cyanosis Related to Pulmonary Diseases
Peripheral cyanosis often manifests in patients with chronic obstructive pulmonary disease (COPD) and pulmonary embolism, where reduced oxygen delivery leads to bluish discoloration of the extremities. This condition is characterized by inadequate peripheral blood oxygenation despite normal central oxygen levels, frequently observed during episodes of hypoxemia in lung pathologies. Early recognition of peripheral cyanosis in pulmonary disease patients is critical for timely intervention and preventing tissue hypoxia complications.
Cyanosis in Chronic Obstructive Pulmonary Disease (COPD)
Cyanosis in Chronic Obstructive Pulmonary Disease (COPD) manifests as a bluish discoloration of the lips, nail beds, and skin due to chronic hypoxemia and impaired oxygen exchange in alveoli. This symptom often indicates advanced emphysema or chronic bronchitis with significant ventilation-perfusion mismatch and elevated levels of deoxygenated hemoglobin. Persistent cyanosis in COPD patients signals the need for supplemental oxygen therapy and reassessment of disease severity to prevent respiratory failure.
Pulmonary Embolism: A Cyanosis Perspective
Pulmonary embolism often presents with sudden onset cyanosis due to impaired oxygen exchange caused by blocked pulmonary arteries. Hypoxemia resulting from ventilation-perfusion mismatch contributes significantly to the bluish discoloration of the skin and mucous membranes. Recognizing cyanosis in pulmonary embolism is crucial for prompt diagnosis and treatment to prevent severe hypoxic injury.
Interstitial Lung Diseases and Their Cyanotic Manifestations
Cyanosis in interstitial lung diseases (ILDs) often results from impaired gas exchange due to fibrosis and inflammation of the lung parenchyma, leading to decreased oxygen saturation. Patients with idiopathic pulmonary fibrosis and sarcoidosis frequently exhibit central cyanosis during exertion or advanced stages, reflecting hypoxemia caused by thickened alveolar-capillary membranes. Pulse oximetry and arterial blood gas analysis are essential diagnostic tools to assess the severity of cyanosis and guide supplemental oxygen therapy in ILD management.
Cyanosis in Acute Respiratory Distress Syndrome (ARDS)
Cyanosis in Acute Respiratory Distress Syndrome (ARDS) manifests as a bluish discoloration of the skin and mucous membranes due to severe hypoxemia caused by impaired gas exchange in damaged alveoli. This condition is characterized by rapid-onset respiratory failure, bilateral pulmonary infiltrates, and refractory hypoxemia despite oxygen therapy. Recognizing central cyanosis in ARDS is critical for timely mechanical ventilation and advanced supportive care to prevent multi-organ dysfunction.
Pediatric Pulmonary Cyanosis: Key Clinical Examples
Pediatric pulmonary cyanosis often presents in congenital heart defects such as Tetralogy of Fallot, characterized by right-to-left shunting and resultant hypoxemia. Other key examples include persistent pulmonary hypertension of the newborn (PPHN), where elevated pulmonary vascular resistance leads to inadequate oxygenation and visible cyanosis. Early recognition of these conditions through clinical signs and pulse oximetry is essential for timely intervention and improved pediatric respiratory outcomes.
Evaluating and Managing Cyanosis in Pulmonary Practice
Cyanosis in pulmonology often indicates underlying hypoxemia caused by conditions such as chronic obstructive pulmonary disease (COPD), pulmonary embolism, or interstitial lung disease. Accurate evaluation involves pulse oximetry, arterial blood gas analysis, and chest imaging to assess oxygenation and identify the primary pulmonary pathology. Management includes supplemental oxygen therapy, treating the root cause, and monitoring for complications to restore adequate tissue oxygenation and prevent progression.
example of cyanosis in pulmonology Infographic
 samplerz.com
samplerz.com