Myelosuppression is a common adverse effect of chemotherapy characterized by the decreased production of blood cells in the bone marrow. For instance, patients receiving cyclophosphamide for breast cancer often experience a significant reduction in white blood cells, red blood cells, and platelets. This suppression leads to increased risks of infection, anemia, and bleeding complications during treatment. Chemotherapeutic agents like methotrexate also frequently induce myelosuppression, especially in patients with lymphoma. Clinical data indicate that neutropenia, a subtype of myelosuppression, occurs in up to 50% of these patients, necessitating dose adjustments and supportive care interventions. Monitoring complete blood counts regularly helps oncologists manage and mitigate the risks associated with myelosuppression in chemotherapy.
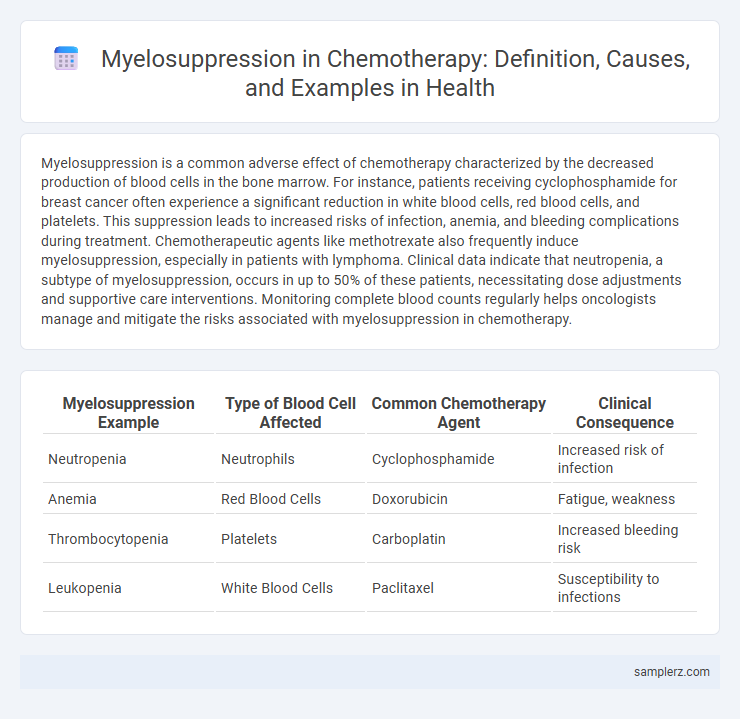
Table of Comparison
| Myelosuppression Example | Type of Blood Cell Affected | Common Chemotherapy Agent | Clinical Consequence |
|---|---|---|---|
| Neutropenia | Neutrophils | Cyclophosphamide | Increased risk of infection |
| Anemia | Red Blood Cells | Doxorubicin | Fatigue, weakness |
| Thrombocytopenia | Platelets | Carboplatin | Increased bleeding risk |
| Leukopenia | White Blood Cells | Paclitaxel | Susceptibility to infections |
Understanding Myelosuppression in Chemotherapy
Myelosuppression is a common adverse effect of chemotherapy, characterized by a significant reduction in bone marrow activity leading to decreased production of blood cells. This condition increases the risk of infections, anemia, and bleeding due to lowered white blood cells, red blood cells, and platelets, respectively. Monitoring complete blood counts regularly during chemotherapy allows for timely management and dose adjustments to mitigate complications associated with myelosuppression.
Common Chemotherapeutic Agents Causing Myelosuppression
Common chemotherapeutic agents causing myelosuppression include cyclophosphamide, doxorubicin, and cisplatin, which significantly reduce bone marrow activity leading to decreased production of blood cells. Methotrexate and paclitaxel also frequently induce myelosuppression by damaging rapidly dividing hematopoietic stem cells. Monitoring blood counts during treatment with these agents is critical to prevent severe neutropenia, anemia, and thrombocytopenia.
Clinical Signs and Symptoms of Myelosuppression
Myelosuppression during chemotherapy manifests through clinical signs such as anemia, leading to fatigue, pallor, and shortness of breath, while neutropenia increases susceptibility to infections characterized by fever and chills. Thrombocytopenia presents with easy bruising, petechiae, and prolonged bleeding. Monitoring complete blood counts is essential for detecting these hematologic toxicities to guide timely intervention.
Real-Life Case Example: Myelosuppression During Cancer Treatment
A 58-year-old female undergoing adjuvant chemotherapy for breast cancer developed severe myelosuppression, characterized by neutropenia and thrombocytopenia, after the third cycle of cyclophosphamide and doxorubicin. This myelosuppressive event necessitated dose reduction and delay in subsequent chemotherapy cycles to allow bone marrow recovery. The case highlights the critical need for regular complete blood count monitoring and supportive care such as granulocyte colony-stimulating factor (G-CSF) to manage chemotherapy-induced myelosuppression effectively.
Laboratory Findings in Myelosuppressed Patients
Myelosuppression in chemotherapy often leads to laboratory findings such as pancytopenia, characterized by decreased levels of white blood cells, red blood cells, and platelets. Common hematologic abnormalities include neutropenia, anemia, and thrombocytopenia, increasing the risk of infections, fatigue, and bleeding. Regular monitoring of complete blood counts (CBC) and differential blood counts is essential to assess bone marrow function and guide treatment adjustments in myelosuppressed patients.
Managing Myelosuppression: Clinical Approaches
Managing myelosuppression in chemotherapy involves proactive use of growth factors like G-CSF to stimulate white blood cell production and reduce infection risk. Dose adjustments and treatment delays are critical strategies to allow bone marrow recovery and minimize severe cytopenias. Regular blood count monitoring enables timely intervention, optimizing patient outcomes and maintaining chemotherapy efficacy.
Risk Factors for Severe Myelosuppression in Chemotherapy
Severe myelosuppression in chemotherapy commonly occurs with high-dose alkylating agents such as cyclophosphamide and platinum-based drugs like cisplatin. Risk factors include advanced age, pre-existing bone marrow disorders, and prolonged prior chemotherapy exposure, which impair hematopoietic recovery. Genetic polymorphisms affecting drug metabolism, combined with poor nutritional status and concurrent infections, further increase vulnerability to severe myelosuppression.
Preventive Strategies to Reduce Myelosuppression
Implementing prophylactic use of colony-stimulating factors like filgrastim effectively reduces the risk of chemotherapy-induced myelosuppression by stimulating white blood cell production. Dose adjustments and treatment schedule modifications are critical preventive strategies to minimize bone marrow suppression while maintaining therapeutic efficacy. Nutritional support and infection control measures further enhance patient outcomes by mitigating complications associated with reduced blood cell counts.
Impact of Myelosuppression on Chemotherapy Schedules
Myelosuppression frequently disrupts chemotherapy schedules by causing significant delays due to decreased bone marrow activity and subsequent reductions in white blood cells, red blood cells, and platelets. These hematologic toxicities elevate the risk of infections, anemia, and bleeding, requiring dose modifications or treatment postponements to ensure patient safety. Maintaining optimal chemotherapy intensity becomes challenging, potentially compromising treatment efficacy and patient outcomes.
Patient Education: Monitoring and Coping with Myelosuppression
Myelosuppression during chemotherapy significantly reduces bone marrow activity, leading to decreased production of blood cells, which increases the risk of infections, anemia, and bleeding complications. Patients should be educated to monitor symptoms such as persistent fatigue, unusual bruising, fever, and frequent infections, and report these signs promptly to healthcare providers for timely intervention. Emphasizing proper hygiene, nutrition, and adherence to prescribed medications helps patients effectively manage myelosuppression and maintain treatment efficacy.
example of myelosuppression in chemotherapy Infographic
 samplerz.com
samplerz.com