Hypochondriasis, also known as illness anxiety disorder, frequently presents in primary care settings where patients exhibit excessive worry about having a serious medical condition despite minimal or no symptoms. These patients often request repeated medical tests and consultations, leading to increased healthcare utilization and anxiety. Family physicians and general practitioners play a crucial role in identifying hypochondriasis by ruling out actual medical conditions and providing reassurance. Data from primary care clinics indicate that hypochondriasis affects approximately 1-5% of patients, highlighting the importance of awareness among healthcare providers. Electronic health records can help track frequent visits and diagnostic tests ordered for these patients, facilitating early detection and management. Behavioral interventions, including cognitive-behavioral therapy, are effective in reducing symptom preoccupation and improving patient quality of life in this population.
Table of Comparison
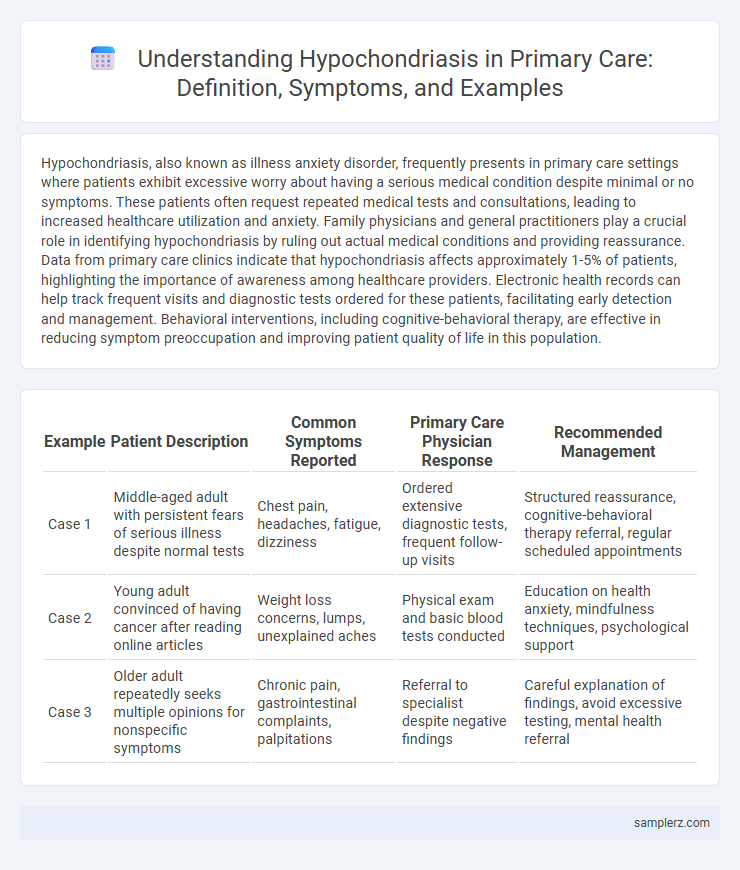
| Example | Patient Description | Common Symptoms Reported | Primary Care Physician Response | Recommended Management |
|---|---|---|---|---|
| Case 1 | Middle-aged adult with persistent fears of serious illness despite normal tests | Chest pain, headaches, fatigue, dizziness | Ordered extensive diagnostic tests, frequent follow-up visits | Structured reassurance, cognitive-behavioral therapy referral, regular scheduled appointments |
| Case 2 | Young adult convinced of having cancer after reading online articles | Weight loss concerns, lumps, unexplained aches | Physical exam and basic blood tests conducted | Education on health anxiety, mindfulness techniques, psychological support |
| Case 3 | Older adult repeatedly seeks multiple opinions for nonspecific symptoms | Chronic pain, gastrointestinal complaints, palpitations | Referral to specialist despite negative findings | Careful explanation of findings, avoid excessive testing, mental health referral |
Understanding Hypochondriasis: Overview and Definition
Hypochondriasis, commonly encountered in primary care, is characterized by excessive preoccupation with having a serious illness despite medical reassurance and lack of significant clinical findings. Patients often report multiple physical symptoms, leading to frequent healthcare visits and diagnostic testing. Early recognition and patient education are crucial to managing this somatic symptom disorder and reducing healthcare utilization.
Common Presentations of Hypochondriasis in Primary Care
Patients with hypochondriasis in primary care often present with persistent concerns about having serious illnesses despite normal diagnostic tests. Common symptoms include frequent visits to healthcare providers, excessive health-related anxiety, and misinterpretation of minor bodily sensations as signs of severe disease. These presentations lead to increased healthcare utilization and challenge clinicians in differentiating hypochondriasis from genuine medical conditions.
Red Flags: Differentiating Hypochondriasis from Physical Illness
In primary care, a key red flag in differentiating hypochondriasis from physical illness is the persistence of excessive health anxiety despite negative medical evaluations and reassurance. Patients with hypochondriasis often exhibit disproportionate concern about minor or nonexistent symptoms, seeking multiple consultations without objective clinical findings. Detailed history and thorough physical examination coupled with appropriate investigations are crucial to rule out organic disease and identify the psychological origin of symptoms.
Case Study: Classic Example of Health Anxiety in Practice
A 34-year-old female repeatedly visited her primary care physician with diverse, unexplained physical complaints, including chest pain and dizziness, despite thorough negative diagnostic tests. Her persistent worry about serious illnesses, such as heart disease or cancer, and preoccupation with bodily sensations exemplify classic health anxiety manifesting as hypochondriasis. This case highlights the importance of recognizing somatic symptom amplification and implementing cognitive-behavioral therapy alongside reassurance in primary care settings.
Impact of Hypochondriasis on Patient-Provider Relationships
Hypochondriasis in primary care often leads to frequent, repetitive visits driven by persistent fears of serious illness despite negative medical evaluations. This disorder can strain patient-provider relationships due to increased provider frustration and challenges in managing healthcare resources efficiently. Effective communication and reassurance strategies are crucial in maintaining trust and ensuring appropriate care for these patients.
Screening Tools for Identifying Hypochondriasis
Screening tools such as the Illness Attitude Scale (IAS) and the Whiteley Index are essential for identifying hypochondriasis in primary care settings, enabling accurate differentiation from other anxiety disorders. The IAS assesses health-related anxiety and disease conviction, while the Whiteley Index measures hypochondriacal beliefs and worries about illness. Implementation of these validated tools improves early detection and guides appropriate intervention for patients exhibiting excessive health concerns.
Evidence-Based Approaches to Diagnosis in Primary Care
Hypochondriasis in primary care is often identified through standardized screening tools such as the Patient Health Questionnaire (PHQ-15) and the Whiteley Index, which assess somatic symptom severity and health anxiety. Evidence-based diagnostic approaches emphasize ruling out organic pathology via targeted clinical evaluation and leveraging cognitive-behavioral therapy (CBT) principles to distinguish hypochondriasis from other medical or psychiatric disorders. Early recognition through validated instruments enhances patient outcomes by guiding appropriate referrals and minimizing unnecessary diagnostic procedures.
Managing Hypochondriasis: Communication Strategies
Effective management of hypochondriasis in primary care involves clear, empathetic communication that validates the patient's concerns while gently guiding them away from excessive medical investigations. Utilizing cognitive-behavioral techniques during consultations helps patients reframe catastrophic health thoughts and reduces unnecessary health anxiety. Establishing regular follow-up appointments fosters trust and provides ongoing support, minimizing the patient's need for urgent visits and reinforcing adherence to treatment plans.
Treatment Options for Hypochondriasis in Primary Care Settings
Treatment options for hypochondriasis in primary care settings include cognitive-behavioral therapy (CBT) aimed at reducing health-related anxiety and maladaptive beliefs. Selective serotonin reuptake inhibitors (SSRIs) are often prescribed to manage associated symptoms such as depression and anxiety. Regular, empathetic follow-up appointments with clear communication help establish trust and reduce unnecessary medical investigations.
Preventing Unnecessary Medical Investigations and Referrals
Hypochondriasis in primary care often presents as excessive worry about having serious illnesses despite normal test results, leading to repeated medical investigations and specialist referrals. Implementing structured clinical assessments and patient education can prevent unnecessary diagnostic procedures and reduce healthcare costs. Early identification and cognitive-behavioral techniques empower patients to manage health anxiety effectively, minimizing overutilization of medical resources.
example of hypochondriasis in primary care Infographic
 samplerz.com
samplerz.com