Stypsis, also known as constipation, is a common gastrointestinal condition characterized by infrequent or difficult bowel movements. This condition may result from a variety of factors including low dietary fiber intake, dehydration, or gastrointestinal motility disorders. Patients often report symptoms such as hard stools, straining during defecation, and a sensation of incomplete evacuation. In clinical settings, stypsis is diagnosed through patient history, physical examination, and sometimes additional tests like colonoscopy or abdominal imaging. Chronic stypsis can lead to complications such as hemorrhoids, fecal impaction, and diverticulosis. Effective management involves dietary modifications, increased fluid intake, and, in some cases, pharmacological treatment like laxatives or prokinetics.
Table of Comparison
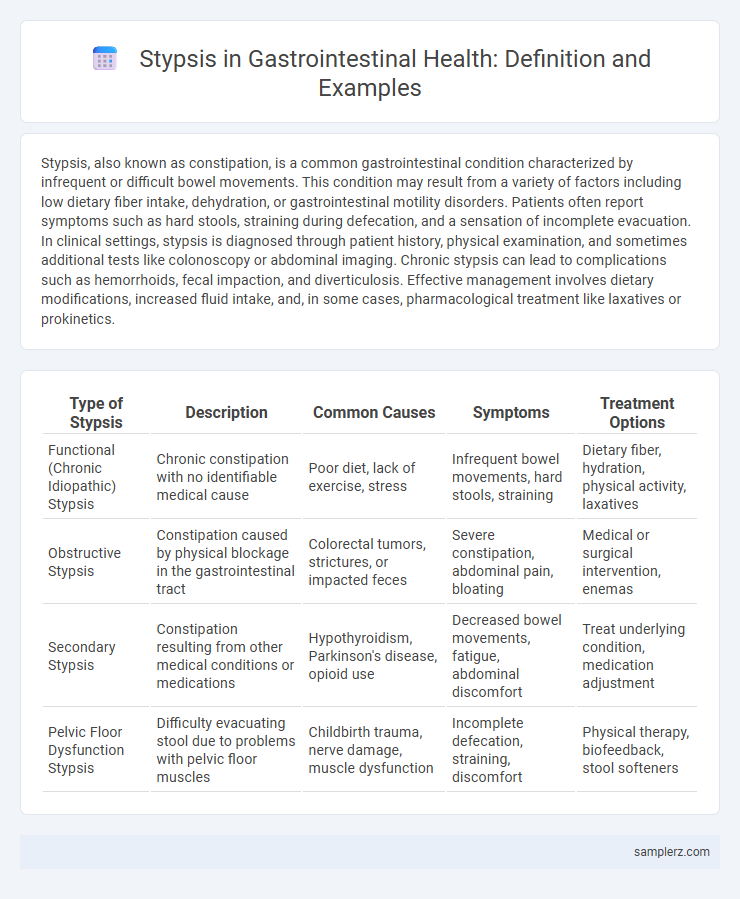
| Type of Stypsis | Description | Common Causes | Symptoms | Treatment Options |
|---|---|---|---|---|
| Functional (Chronic Idiopathic) Stypsis | Chronic constipation with no identifiable medical cause | Poor diet, lack of exercise, stress | Infrequent bowel movements, hard stools, straining | Dietary fiber, hydration, physical activity, laxatives |
| Obstructive Stypsis | Constipation caused by physical blockage in the gastrointestinal tract | Colorectal tumors, strictures, or impacted feces | Severe constipation, abdominal pain, bloating | Medical or surgical intervention, enemas |
| Secondary Stypsis | Constipation resulting from other medical conditions or medications | Hypothyroidism, Parkinson's disease, opioid use | Decreased bowel movements, fatigue, abdominal discomfort | Treat underlying condition, medication adjustment |
| Pelvic Floor Dysfunction Stypsis | Difficulty evacuating stool due to problems with pelvic floor muscles | Childbirth trauma, nerve damage, muscle dysfunction | Incomplete defecation, straining, discomfort | Physical therapy, biofeedback, stool softeners |
Overview of Stypsis in the Gastrointestinal Tract
Stypsis, commonly known as constipation, in the gastrointestinal tract is characterized by infrequent bowel movements, hard stool consistency, and difficulty during defecation. This condition often results from slowed colonic transit or impaired rectal evacuation, affecting millions globally, with prevalence higher in elderly and sedentary populations. Dietary fiber deficiency, dehydration, and certain medications are primary contributors to stypsis, necessitating targeted lifestyle and pharmacologic interventions.
Common Causes of Gastrointestinal Stypsis
Common causes of gastrointestinal stypsis include inadequate dietary fiber intake, dehydration, and insufficient physical activity. Conditions such as irritable bowel syndrome (IBS), hypothyroidism, and certain medications like opioids and antacids can also contribute to persistent constipation. Structural abnormalities, including strictures or colorectal cancer, should be considered in chronic or severe cases of stypsis.
Clinical Manifestations of GI Stypsis
Gastrointestinal stypsis, commonly known as constipation, presents clinically with infrequent bowel movements typically fewer than three per week, hard or lumpy stools, and difficulty during defecation. Patients often report abdominal discomfort, bloating, and a sensation of incomplete evacuation. Physical examination may reveal abdominal distension and reduced bowel sounds, while digital rectal examination can identify impacted fecal masses.
Types of Constipation Seen in GI Disorders
Chronic idiopathic constipation often presents with infrequent bowel movements and hard stools, distinguishing it from slow-transit constipation characterized by delayed colonic transit time due to motility dysfunction. Outlet obstruction constipation arises from pelvic floor dyssynergia, where impaired relaxation of pelvic muscles inhibits stool evacuation. Secondary constipation may result from underlying gastrointestinal disorders such as irritable bowel syndrome or metabolic causes like hypothyroidism, impacting bowel regularity.
Diagnostic Approaches to Stypsis in the GI System
Diagnostic approaches to stypsis in the gastrointestinal system often involve comprehensive patient history and physical examination to identify underlying causes such as dietary habits or medication use. Advanced techniques include colonoscopy to visualize colonic mucosa, anorectal manometry for evaluating sphincter function, and imaging studies like abdominal X-rays or CT scans to detect obstructions or structural abnormalities. Laboratory tests assessing stool consistency, blood presence, and inflammatory markers further aid in distinguishing between functional constipation and secondary pathologies.
Dietary Factors Influencing GI Stypsis
Dietary factors significantly influence gastrointestinal stypsis, with low fiber intake being a primary contributor to constipation. Insufficient consumption of fruits, vegetables, and whole grains reduces stool bulk and slows colonic transit time. Inadequate hydration and high intake of processed foods and dairy products further exacerbate symptoms by promoting harder stool consistency.
Medical Conditions Associated with GI Stypsis
GI stypsis, commonly known as constipation, is frequently associated with medical conditions such as irritable bowel syndrome (IBS), hypothyroidism, and diabetes mellitus. Neurological disorders like Parkinson's disease and multiple sclerosis often contribute to impaired bowel motility leading to persistent stypsis. Medication side effects, including opioids and anticholinergics, also exacerbate gastrointestinal transit delays resulting in chronic constipation.
Pharmacological Treatments for GI Stypsis
Pharmacological treatments for gastrointestinal stypsis primarily include laxatives such as osmotic agents (polyethylene glycol and lactulose) that increase water content in the stool, stimulant laxatives (bisacodyl and senna) that enhance intestinal motility, and stool softeners like docusate sodium that facilitate easier defecation. Prokinetic agents, including prucalopride, are prescribed to improve colonic transit in chronic constipation unresponsive to standard laxatives. Prescription medications target underlying pathophysiology to relieve symptoms effectively while minimizing adverse effects in patients with stypsis.
Non-Pharmacological Management Strategies
Stypsis, characterized by severe constipation often stemming from gastrointestinal motility disorders, can be effectively managed through non-pharmacological strategies. Key approaches include increasing dietary fiber intake, ensuring adequate hydration, and encouraging regular physical activity to stimulate bowel movements. Incorporating behavioral modifications such as scheduled toileting and stress reduction techniques further supports gastrointestinal health and improves stool consistency.
Prevention and Long-Term Management of GI Stypsis
Chronic stypsis in the gastrointestinal tract can be effectively prevented and managed through a high-fiber diet rich in fruits, vegetables, and whole grains, which enhances bowel motility and stool bulk. Adequate hydration and regular physical activity support intestinal function and reduce the risk of recurrent constipation. Long-term management may also involve the use of osmotic laxatives or stool softeners under medical supervision to maintain consistent bowel movements and prevent complications such as hemorrhoids or fecal impaction.
example of stypsis in gastrointestinal Infographic
 samplerz.com
samplerz.com