Polypharmacy in geriatric care refers to the use of multiple medications by elderly patients, often to manage several chronic conditions simultaneously. An example includes an 80-year-old patient prescribed medications such as antihypertensives for high blood pressure, antidiabetics for type 2 diabetes, and anticoagulants for atrial fibrillation. This combination highlights the complexity of managing different health issues while minimizing drug interactions and adverse effects. Geriatric patients frequently receive medications from different healthcare providers, which increases the risk of polypharmacy-related complications. Data shows that 40% of elderly individuals take five or more prescription drugs daily, leading to potential issues such as increased hospitalizations and cognitive decline. Careful medication review and management are crucial to optimizing health outcomes in this population.
Table of Comparison
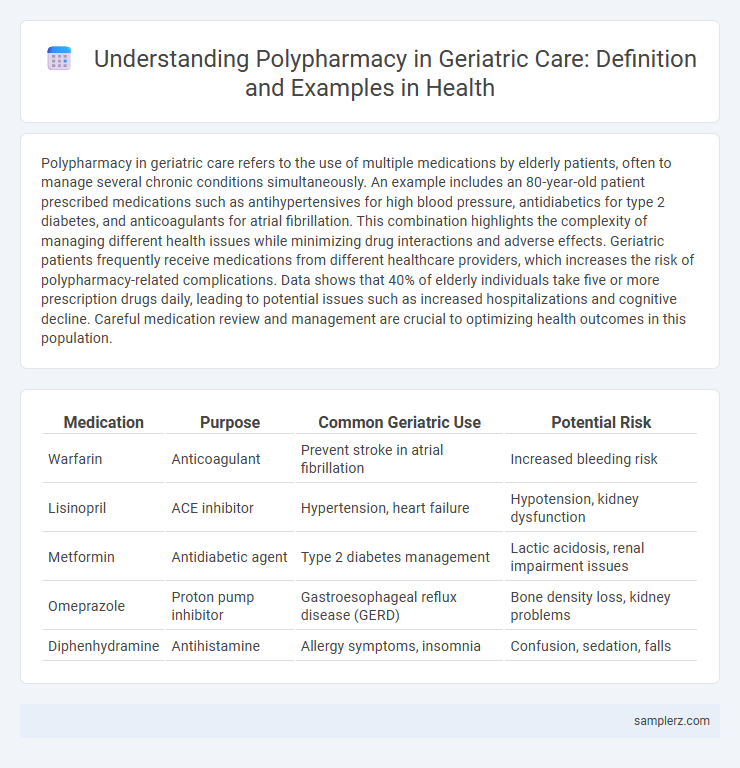
| Medication | Purpose | Common Geriatric Use | Potential Risk |
|---|---|---|---|
| Warfarin | Anticoagulant | Prevent stroke in atrial fibrillation | Increased bleeding risk |
| Lisinopril | ACE inhibitor | Hypertension, heart failure | Hypotension, kidney dysfunction |
| Metformin | Antidiabetic agent | Type 2 diabetes management | Lactic acidosis, renal impairment issues |
| Omeprazole | Proton pump inhibitor | Gastroesophageal reflux disease (GERD) | Bone density loss, kidney problems |
| Diphenhydramine | Antihistamine | Allergy symptoms, insomnia | Confusion, sedation, falls |
Understanding Polypharmacy in Geriatric Patients
Polypharmacy in geriatric care refers to the use of multiple medications, often five or more, to manage chronic conditions such as hypertension, diabetes, and arthritis common in elderly patients. This practice increases the risk of adverse drug reactions, drug interactions, and medication non-adherence, complicating overall treatment effectiveness. Healthcare providers must conduct regular medication reviews to optimize drug regimens and ensure patient safety in this vulnerable population.
Common Drug Combinations in Elderly Care
Common drug combinations in geriatric care often include antihypertensives with diuretics, anticoagulants alongside antiplatelet agents, and antidiabetics combined with statins to manage multiple chronic conditions. Polypharmacy increases the risk of adverse drug reactions, drug-drug interactions, and medication non-adherence among elderly patients. Monitoring and regular medication reviews are essential to optimize therapeutic outcomes and minimize potential harms in this population.
Risk Factors Leading to Polypharmacy Among Seniors
Multiple chronic conditions such as hypertension, diabetes, and arthritis significantly increase the risk of polypharmacy among seniors, leading to the simultaneous use of five or more medications. Cognitive decline and lack of coordination between multiple healthcare providers exacerbate medication discrepancies and adverse drug interactions. Limited access to comprehensive medication reviews and insufficient patient education further contribute to inappropriate medication use in geriatric care.
Clinical Consequences of Polypharmacy in Older Adults
Polypharmacy in geriatric care often leads to increased risks of adverse drug reactions, drug-drug interactions, and medication non-adherence among older adults. Clinical consequences include heightened incidence of falls, cognitive impairment, hospitalization, and functional decline. Careful medication reconciliation and regular review are essential to mitigate these risks and improve patient outcomes.
Case Study: Polypharmacy in a Geriatric Patient
A geriatric patient aged 78 with multiple chronic conditions including hypertension, diabetes, and osteoarthritis was prescribed over eight medications leading to increased risk of adverse drug reactions and medication non-adherence. This case study highlights the importance of comprehensive medication review and deprescribing strategies to minimize polypharmacy-related complications. Regular follow-up and interdisciplinary collaboration improved the patient's quality of life by optimizing pharmacotherapy and reducing drug interactions.
Drug-Drug Interactions Frequently Observed in the Elderly
Polypharmacy in geriatric care often leads to drug-drug interactions such as increased bleeding risk from concurrent use of anticoagulants like warfarin and antiplatelet agents. Elderly patients commonly experience adverse interactions between benzodiazepines and opioids, heightening sedation and respiratory depression risks. Monitoring pharmacokinetic changes due to age-related renal and hepatic function decline is crucial to prevent toxicity and therapeutic failures.
Strategies for Safe Medication Management in Geriatrics
Polypharmacy in geriatric care often involves the simultaneous use of five or more medications, increasing risks of adverse drug reactions and drug interactions among elderly patients. Strategies for safe medication management include comprehensive medication reviews by healthcare professionals, use of electronic prescribing systems, and employing deprescribing protocols to minimize unnecessary medications. Implementing tailored care plans and regular monitoring enhances patient adherence and reduces hospitalizations due to medication-related complications.
The Role of Healthcare Teams in Reducing Polypharmacy
Healthcare teams play a critical role in reducing polypharmacy among geriatric patients by conducting comprehensive medication reviews and coordinating care across multiple providers. Pharmacists, physicians, and nurses collaborate to identify potentially inappropriate medications, optimize drug regimens, and monitor for adverse drug interactions common in elderly populations. This multidisciplinary approach improves patient safety, reduces hospitalizations, and enhances overall quality of life for older adults managing multiple chronic conditions.
Deprescribing Approaches in Geriatric Care
Polypharmacy in geriatric care often involves multiple medications for chronic conditions such as hypertension, diabetes, and arthritis, increasing the risk of adverse drug reactions and hospitalizations. Deprescribing approaches focus on systematically reviewing each medication to evaluate its current necessity, potential side effects, and interactions, with the goal of minimizing polypharmacy and improving patient outcomes. Tools like the Beers Criteria and STOPP/START guidelines support clinicians in identifying potentially inappropriate medications for older adults.
Monitoring and Review Practices for Polypharmacy in Seniors
Effective monitoring and review practices for polypharmacy in geriatric care involve regular medication reconciliation, comprehensive assessment of drug interactions, and evaluation of therapy appropriateness. Clinical tools like the Beers Criteria and STOPP/START criteria guide prescribers in minimizing potentially inappropriate medications in seniors. Ongoing collaboration among healthcare providers, pharmacists, and caregivers ensures timely identification of adverse drug events and optimization of medication regimens to enhance safety and efficacy.
example of Polypharmacy in geriatric care Infographic
 samplerz.com
samplerz.com