Telehealth in rural clinics has transformed healthcare delivery by enabling remote consultations and access to specialists. Patients in isolated areas can receive timely diagnoses and treatment plans through video conferencing technology. This approach reduces travel time and increases medical care accessibility for underserved populations. Data indicates that rural clinics equipped with telehealth services experience improved patient outcomes and higher appointment adherence rates. Entities such as primary care providers, mental health specialists, and pharmacists collaborate virtually to offer comprehensive care. Implementing telehealth technology reduces healthcare costs while expanding the clinical capabilities of rural healthcare facilities.
Table of Comparison
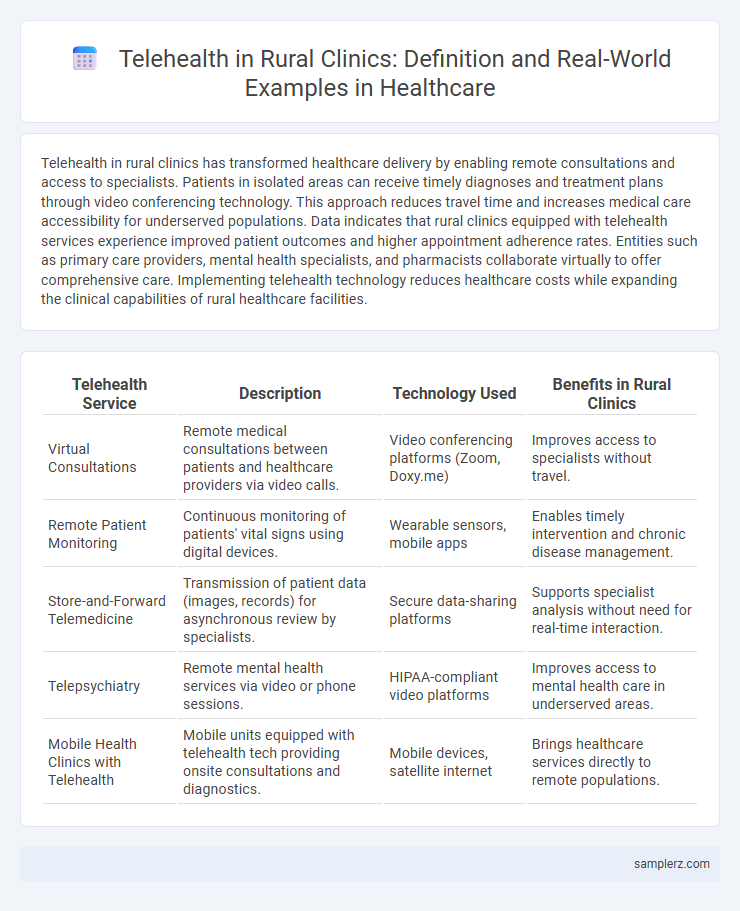
| Telehealth Service | Description | Technology Used | Benefits in Rural Clinics |
|---|---|---|---|
| Virtual Consultations | Remote medical consultations between patients and healthcare providers via video calls. | Video conferencing platforms (Zoom, Doxy.me) | Improves access to specialists without travel. |
| Remote Patient Monitoring | Continuous monitoring of patients' vital signs using digital devices. | Wearable sensors, mobile apps | Enables timely intervention and chronic disease management. |
| Store-and-Forward Telemedicine | Transmission of patient data (images, records) for asynchronous review by specialists. | Secure data-sharing platforms | Supports specialist analysis without need for real-time interaction. |
| Telepsychiatry | Remote mental health services via video or phone sessions. | HIPAA-compliant video platforms | Improves access to mental health care in underserved areas. |
| Mobile Health Clinics with Telehealth | Mobile units equipped with telehealth tech providing onsite consultations and diagnostics. | Mobile devices, satellite internet | Brings healthcare services directly to remote populations. |
Introduction to Telehealth in Rural Clinics
Telehealth in rural clinics enables remote diagnosis, consultation, and treatment through video conferencing and mobile health applications, bridging the gap in healthcare access. This technology reduces travel time for patients in underserved areas, improving chronic disease management and follow-up care. Rural telehealth programs also incorporate remote patient monitoring tools to enhance real-time data collection and clinical decision-making.
Key Benefits of Telehealth for Rural Communities
Telehealth in rural clinics significantly improves access to specialized healthcare services, reducing travel time for patients by up to 75%. This technology enhances chronic disease management by enabling regular remote monitoring and timely interventions, leading to better health outcomes. Cost savings from telehealth also alleviate financial burdens on rural healthcare facilities and patients alike, promoting sustainable healthcare delivery.
Common Telehealth Technologies Used in Rural Healthcare
Common telehealth technologies used in rural healthcare include video conferencing platforms, remote patient monitoring devices, and mobile health applications, which enable real-time consultations and continuous health data tracking. These tools facilitate access to specialty care, reduce travel time for patients, and enhance chronic disease management in underserved rural populations. Integration of electronic health records with telehealth systems further improves coordinated care and clinical decision-making in rural clinics.
Virtual Consultations for Chronic Disease Management
Virtual consultations in rural clinics enable patients with chronic diseases to receive timely medical advice without traveling long distances, improving access to care. Through telehealth platforms, healthcare providers can monitor conditions like diabetes, hypertension, and COPD remotely, adjusting treatments based on real-time patient data. This approach reduces hospital admissions and enhances disease management efficiency in underserved rural populations.
Remote Patient Monitoring in Rural Health Settings
Remote Patient Monitoring (RPM) in rural clinics enhances chronic disease management by continuously tracking patients' vital signs and transmitting data to healthcare providers. This technology reduces hospital visits and enables timely interventions for conditions like diabetes and hypertension in underserved areas. RPM improves care access by overcoming geographical barriers, ultimately leading to better health outcomes in rural populations.
Telepsychiatry Services in Underserved Areas
Telepsychiatry services in rural clinics provide vital mental health support to underserved areas by connecting patients with licensed psychiatrists through secure video conferencing platforms. This approach reduces travel barriers and increases access to timely psychiatric evaluations, medication management, and therapy for populations facing geographic and resource limitations. Studies show telepsychiatry improves treatment adherence and mental health outcomes in rural communities lacking in-person psychiatric care.
Maternal and Pediatric Telehealth Examples
Rural clinics utilize telehealth platforms such as video consultations for prenatal checkups and remote fetal monitoring to enhance maternal care. Pediatric telehealth services include virtual well-child visits and remote management of chronic conditions like asthma, improving access to specialized care in underserved areas. Integration of electronic health records with telehealth systems allows seamless coordination between rural clinics and urban specialists, optimizing maternal and pediatric health outcomes.
Overcoming Connectivity Challenges in Rural Clinics
Telehealth in rural clinics leverages satellite internet and mobile broadband technologies to overcome connectivity challenges, enabling real-time video consultations and remote monitoring for patients. Implementation of store-and-forward systems allows healthcare providers to exchange patient data asynchronously, reducing dependence on continuous high-speed internet. These innovations significantly improve access to specialist care and health outcomes in underserved rural communities.
Case Studies: Successful Telehealth Implementations
Rural clinics have successfully implemented telehealth solutions such as the Cherokee Health Systems model, which increased patient access to specialty care and reduced travel time by 40%. The Veterans Health Administration's telehealth program demonstrated a 25% reduction in hospital readmissions among rural veterans through remote monitoring and virtual consultations. These case studies highlight telehealth's role in overcoming geographical barriers and improving health outcomes in underserved rural populations.
The Future of Telehealth in Rural Healthcare Delivery
Telehealth in rural clinics is revolutionizing healthcare delivery by providing remote access to specialists, reducing patient travel time, and enabling continuous monitoring through wearable technology. Advanced telecommunication infrastructure supports real-time consultations, diagnostic imaging, and electronic health records integration, enhancing care coordination. Emerging trends in artificial intelligence and remote patient monitoring devices promise to further bridge the healthcare gap in underserved rural populations.
example of telehealth in rural clinic Infographic
 samplerz.com
samplerz.com