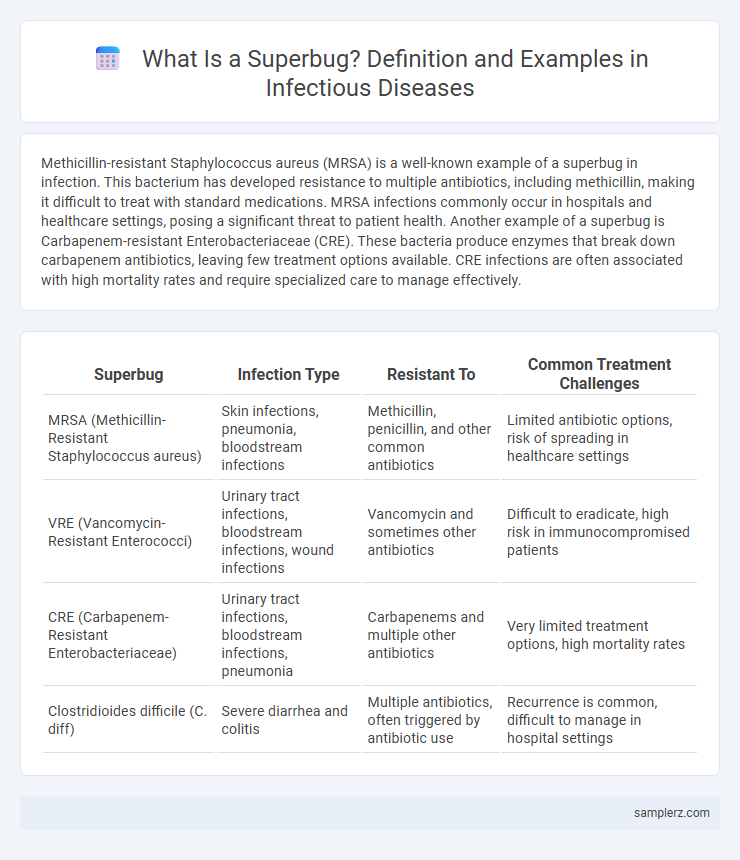
Methicillin-resistant Staphylococcus aureus (MRSA) is a well-known example of a superbug in infection. This bacterium has developed resistance to multiple antibiotics, including methicillin, making it difficult to treat with standard medications. MRSA infections commonly occur in hospitals and healthcare settings, posing a significant threat to patient health. Another example of a superbug is Carbapenem-resistant Enterobacteriaceae (CRE). These bacteria produce enzymes that break down carbapenem antibiotics, leaving few treatment options available. CRE infections are often associated with high mortality rates and require specialized care to manage effectively.
Table of Comparison
| Superbug | Infection Type | Resistant To | Common Treatment Challenges |
|---|---|---|---|
| MRSA (Methicillin-Resistant Staphylococcus aureus) | Skin infections, pneumonia, bloodstream infections | Methicillin, penicillin, and other common antibiotics | Limited antibiotic options, risk of spreading in healthcare settings |
| VRE (Vancomycin-Resistant Enterococci) | Urinary tract infections, bloodstream infections, wound infections | Vancomycin and sometimes other antibiotics | Difficult to eradicate, high risk in immunocompromised patients |
| CRE (Carbapenem-Resistant Enterobacteriaceae) | Urinary tract infections, bloodstream infections, pneumonia | Carbapenems and multiple other antibiotics | Very limited treatment options, high mortality rates |
| Clostridioides difficile (C. diff) | Severe diarrhea and colitis | Multiple antibiotics, often triggered by antibiotic use | Recurrence is common, difficult to manage in hospital settings |
Understanding Superbugs: An Overview
Methicillin-resistant Staphylococcus aureus (MRSA) exemplifies a superbug causing severe infections resistant to multiple antibiotics, complicating treatment protocols. These bacteria have evolved mechanisms such as producing altered penicillin-binding proteins, rendering many standard antibiotics ineffective. Understanding the genetic mutations and environmental factors that contribute to MRSA resistance is crucial for developing advanced therapies and infection control strategies.
MRSA: The Hospital-Acquired Superbug
MRSA (Methicillin-Resistant Staphylococcus aureus) is a prime example of a hospital-acquired superbug responsible for severe infections that are difficult to treat due to resistance to multiple antibiotics. This pathogen commonly causes bloodstream infections, pneumonia, and surgical site infections in healthcare settings, posing significant risks to immunocompromised patients. Effective infection control measures and antibiotic stewardship are crucial to limiting the spread of MRSA within hospitals.
CRE: The Rise of Carbapenem-Resistant Enterobacteriaceae
Carbapenem-Resistant Enterobacteriaceae (CRE) are a critical example of superbugs causing severe healthcare-associated infections worldwide. These bacteria exhibit resistance to carbapenems, potent antibiotics often reserved as last-resort treatments for multidrug-resistant infections. CRE infections lead to higher morbidity, mortality rates, and limited therapeutic options, posing significant challenges to infection control and antibiotic stewardship programs.
Clostridioides difficile: A Dangerous Health Care Superbug
Clostridioides difficile, often abbreviated as C. difficile, is a notorious superbug responsible for severe healthcare-associated infections, particularly antibiotic-associated diarrhea and colitis. Its ability to form resilient spores makes it difficult to eliminate in hospital environments, leading to recurrent infections and increased morbidity. Effective infection control measures and targeted antibiotic stewardship are crucial to combat the rising threat posed by C. difficile within healthcare settings.
VRE: Vancomycin-Resistant Enterococci in Infections
Vancomycin-Resistant Enterococci (VRE) represent a critical superbug in healthcare-associated infections, exhibiting resistance to vancomycin, a last-resort antibiotic. VRE primarily causes bloodstream infections, urinary tract infections, and surgical site infections, posing significant treatment challenges. Its prevalence in hospital environments underscores the urgent need for stringent infection control and antimicrobial stewardship strategies.
Multidrug-Resistant Tuberculosis (MDR-TB) Threat
Multidrug-Resistant Tuberculosis (MDR-TB) represents a critical public health challenge due to its resistance to at least isoniazid and rifampicin, the two most potent first-line anti-TB drugs. The World Health Organization estimates that approximately 450,000 new cases of MDR-TB emerge globally each year, complicating treatment outcomes and increasing mortality rates. Effective management requires specialized second-line drug regimens, prolonged therapy, and robust diagnostic capabilities to combat the threat posed by this superbug strain.
ESBL-Producing Bacteria: A Growing Concern
ESBL-producing bacteria, such as Escherichia coli and Klebsiella pneumoniae, are a significant cause of antibiotic-resistant infections worldwide. These pathogens produce extended-spectrum beta-lactamases (ESBLs) that degrade critical antibiotics like penicillins and cephalosporins, complicating treatment options. The increasing prevalence of ESBL-producing bacteria in healthcare settings poses a serious challenge to infection control and patient outcomes.
Acinetobacter baumannii: The Opportunistic Superbug
Acinetobacter baumannii represents a notorious opportunistic superbug commonly responsible for multidrug-resistant infections in healthcare settings, particularly ventilator-associated pneumonia and bloodstream infections. This pathogen thrives in intensive care units, demonstrating resistance to carbapenems, colistin, and other last-resort antibiotics, complicating treatment protocols. Its ability to form biofilms on medical devices and surfaces exacerbates infection control challenges, making Acinetobacter baumannii a critical target for antimicrobial stewardship and infection prevention strategies.
Gonorrhea and Its Resistance to Antibiotics
Gonorrhea, caused by the bacterium Neisseria gonorrhoeae, is a prominent example of a superbug due to its increasing resistance to multiple antibiotics, including cephalosporins and fluoroquinolones. The rapid emergence of strains resistant to extended-spectrum cephalosporins such as ceftriaxone has significantly complicated treatment protocols and heightened concerns about untreatable infections. Surveillance data from the Centers for Disease Control and Prevention (CDC) underscore the urgent need for novel therapeutic strategies and enhanced antibiotic stewardship to combat multidrug-resistant gonorrhea effectively.
Preventive Measures Against Superbug Infections
Methicillin-resistant Staphylococcus aureus (MRSA) represents a prominent superbug causing severe infections resistant to multiple antibiotics. Preventive measures include strict hand hygiene protocols, regular disinfection of hospital environments, and prudent antibiotic stewardship to limit resistance development. Using personal protective equipment (PPE) and isolating infected patients further help reduce the transmission of superbug infections in healthcare settings.
example of superbug in infection Infographic
 samplerz.com
samplerz.com